Endovascular repair techniques for diseases affecting the descending thoracic aorta1 are often used as an alternative to surgery, particularly in older patients and those with associated diseases, because of the lower morbidity and mortality of these procedures.2 The reported long-term outcome of endovascular repair varies considerably among studies. The most commonly described complication is detection of endoleaks, which are defined as persistent arterial flow external to the stent-graft lumen. Although the diagnosis has been traditionally established by digital subtraction angiography, computed tomography, which tends to be the initial diagnostic technique used in these aortic diseases, is increasingly being employed for long-term follow-up of these patients.3
We carried out a study to determine the presence and types of late endoleaks in descending aorta stent-grafts by multidetector computed tomography.
This study included 36 patients (32 men) with a mean age of 63 (36-83) years, who underwent endovascular stent grafting of the descending aorta between January 2008 and January 2011, and had more than 1 year of multidetector computed tomography follow-up.
Endovascular treatment was performed for the following indications: aortic aneurysms (14 patients), type B aortic dissection (16 patients), intramural hematoma associated with a penetrating aortic ulcer (5 patients), and traumatic aortic rupture (1 patient).
A 64-detector computed tomography unit was used, and the study covered the entire thorax and abdomen in 2 acquisitions. The first was performed without contrast and the second was contrast-enhanced in the arterial phase to identify calcifications that could simulate an endoleak because of their high radiologic density. In addition to the usual axial, coronal, and oblique views, multiplanar recontruction (MPR), maximum intensity projection (MIP) and 3-dimensional virtual recontructions (3D-VR) were performed. In all patients, an advanced analysis of the vessel was carried out, calculating the area and diameters of the entire aorta in slices perpendicular to its longitudinal axis. When required, the vessel section was corrected manually (as in cases of thrombosed aneurysms) to include the area that had been excluded and to assess possible growth.
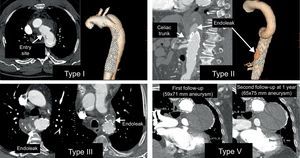
We analyzed the presence of 4 of the 5 types of endoleaks described:4 type I, deficient sealing of the stent-graft (proximal or distal neck); type II, retrograde flow through collateral vessels; type III, structural changes in the stent-graft (breakage or modular separation); and type V, endotension (expansion of a thrombosed aneurysm without evidence of endoleak formation). Type IV endoleak (porosity) was not included, being a rare, transient endoleak that is detected on invasive arteriography.
Endoleaks were detected in 9 (25%) of the 36 patients. In 8 patients, type I, II and III endoleaks were seen on the first multidetector computed tomography study following stent-graft implantation (1-6 months) and in 1 patient, a type V endoleak was demonstrated at the 1-year follow-up, with continuous expansion in successive studies.
Type 1 endoleaks were observed in 4 patients with aortic dissection; type II, in 1 patient with an aneurysm; type III, in 3 patients with an aneurysm; and type V, in 1 patient, also with an aneurysm (Figure).
Type I endoleak: Dissection of the descending aorta with defective sealing of the proximal portion of the stent-graft. Type II endograft: With repatency of the aneurysmal sac through the celiac trunk, which was occluded at its origin, with filling through collateral vessels from the superior mesenteric artery. Type III endoleak: 2 cases with contrast passage to the aneurysm due to a structural stent-graft alteration. Type V endoleak: Expansion of a thrombosed aneurysm at the follow-up examination, without evidence of a leak.
Endoleaks are the most common late complications of endovascular repair of the descending aorta, with a reported incidence reaching 30% and a mean incidence of 13%.5 The incidence in our study was 25%.
Type I endoleak tends to occur in patients whose underlying aortic disease is a dissection and the communication between the true and false lumen persists. Type II endoleak usually occurs in patients treated for an aortic aneurysm, and consists of repatency of the aneurysmal sac by collateral vessels. In our single case of this type of endoleak, the collateral originated from branches of the superior mesenteric artery that filled the proximal portion of the celiac trunk (occluded by the stent-graft, which covered the distal third of the descending thoracic aorta and the upper third of the abdominal aorta). Type III endoleak usually occurs in patients treated for an aortic aneurysm. In addition to structural failure of the stent-graft, the stress that the stent sustains due to aortic pulsatility or constriction of the aneurysmal sac can facilitate the development of endoleak. Type V endoleak consists of gradual expansion of the aneurysmal sac without an obvious endoleak.
In conclusion, endoleaks are common following endovascular treatment of the descending aorta, and their noninvasive follow-up with multidetector computed tomography study is a feasible approach.
.