Coronary obstruction is reported in 1% of transcatheter aortic valve implantation (TAVI) procedures, making it a dreaded complication.1 According to a large study, the vast majority of cases (89%) become manifest during the procedure.2 We report the cases of 2 patients that illustrate how coronary obstruction can occur several hours after implantation of self-expandable valves.
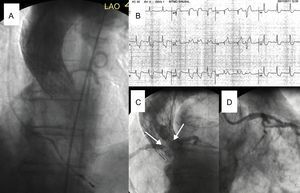
The first patient was an 87-year-old woman in a delicate state of health with bronchial asthma. She was scheduled for transfemoral TAVI (Society of Thoracic Surgeons score, 6%). The echocardiographic study showed a moderately calcified valve with maximum gradient of 81mmHg, mean gradient of 40mmHg, and area of 0.9cm2. The aortic root was small (annulus diameter, 21mm; sinus, 24mm; height of the left ostium, 6mm). After 18mm balloon valvuloplasty with simultaneous aortography, a 26mm CoreValve was implanted. The positioning was high but the functional result was acceptable (Figure 1 and video 1 of the supplementary material). The next day, the patient developed angina with ST depression. Aortography showed preserved coronary artery flow, and therefore it was decided to start medical treatment. Three days later, she had a more intense episode with diffuse ST depression. Coronary angiography showed that the skirt of the prosthesis had compromised both ostia (video 2 of the supplementary material). The patient went into cardiorespiratory arrest, which resolved with resuscitation measures, balloon contrapulsation, and retraction with a 20mm snare catheter (video 3 of the supplementary material). The patency of the coronary arteries was then confirmed (video 4 of the supplementary material) and an improvement was observed in the maximum gradient (49mmHg). The patient refused any additional procedures and was discharged. She remained free of events for 24 months.
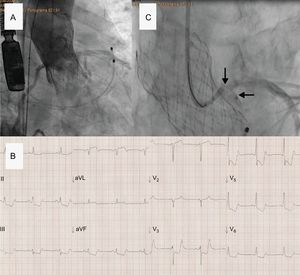
The second patient was an 81-year-old man with limited mobility and a history of myocardial infarction. He presented with myelofibrosis with severe pancytopenia and critical aortic stenosis (maximum gradient, 107mmHg; mean, 63mmHg; area, 0.5cm2), with severe leaflet calcification (Society of Thoracic Surgeons score, 6%). Computed tomography showed an annulus with a mean diameter of 23mm, and derived from the perimeter, a left sinus of 29mm and a left ostium with a height of 9mm. Transfemoral TAVI was programmed under heparin treatment, single antiplatelet therapy with aspirin, and prior platelet transfusion. After 23mm balloon valvuloplasty, a 29mm Evolut R valve was implanted, with postdilation using a 25 balloon (Figure 2 and video 5 of the supplementary material). At 2hours after arrival in the intensive care unit, the patient experienced repeated episodes of angina with diffuse ST depression. Coronary angiography showed subocclusion of the trunk by a large calcified mass corresponding to the displaced native valve leaflet (video 6 of the supplementary material). Given the appropriate position and acceptable clinical tolerance, retraction was ruled out and the patient underwent percutaneous coronary intervention. After repeat attempts to pass through the obstruction, we decided to perform surgical revascularization. During transfer to surgery, the patient experienced a cardiac arrest.
The main mechanism of coronary obstruction associated with TAVI is displacement of the thickened and calcified native valve over the coronary ostium. Another much less frequent mechanism is direct obstruction by the prosthesis skirt.3 In addition, other dynamic processes may be present such as tissue hematoma,4 stasis of the aortic sinus,5 and gradual expansion after implantation of self-expandable valves,6 thus explaining the different presentations of the complication.
In a multicenter study of 6688 TAVI procedures, Ribeiro et al.2 identified height of the left ostium < 12mm and sinus diameter < 30mm as the most important predictors of risk of obstruction from the anatomical point of view. In cases of higher risk, certain measures may help avoid the onset of such complications. These include adjusting the size of the valve to the outer annulus (for example, 26mm instead of 29mm in the second patient); avoiding implantation in a high position, thereby reducing the remaining space and favoring blood stasis; assessing behavior during valvuloplasty, although the sensitivity of this maneuver may be reduced when small balloons are used; and protecting the coronary artery during implantation with a high-support guidewire, thereby allowing the alignment to be changed and facilitating access if there is obstruction.
The usual treatment is a percutaneous coronary intervention,2 but sometimes the guidewire cannot be advanced. In these cases, retraction toward the ascending aorta is a reasonable alternative. This maneuver can be performed with a snare catheter or, as an emergency resource, with an oversized balloon at the waist of the prosthesis.3
In conclusion, late obstruction of the coronary ostium is a potential complication in the first few hours after implantation of self-expandable valves. Identification of associated factors is essential for the prevention and early diagnosis of this complication.
CONFLICTS OF INTERESTC. Morís is a consultant for Medtronic for implantation of CoreValve percutaneous aortic prostheses.