Fontan palliation was first described for the treatment of tricuspid atresia, but the indications have since been extended to other complex congenital defects such as univentricular hearts.1 Since the original atriopulmonary connection procedure—which was associated with a high incidence of atrial arrhythmias, among other disadvantages—the technique has been improved and extracardiac cavopulmonary connection is currently used.1 This approach is simple, the hemodynamic outcomes are excellent, and the percentage of arrhythmias during follow-up is low.2 However, atrial arrhythmias are not completely eliminated and the venous access routes to the heart are lacking, making percutaneous techniques much more difficult to carry out.
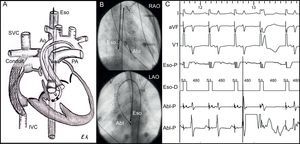
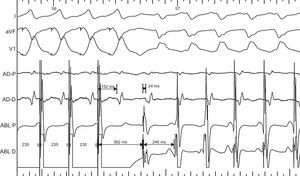
We report the case of a 4-year-old boy weighing 19.5kg, who had a univentricular heart due to tricuspid atresia. The position of the great vessels was normal, and there was an obstructive bulboventricular foramen. He had undergone a bidirectional Glenn procedure and ligation of the pulmonary artery when aged 2 years. Subsequently, extracardiac Fontan palliation was performed. Three months after the last intervention, he started to experience episodes of supraventricular tachycardia, with poor hemodynamic tolerance, which required repeated admission to the emergency room. The episodes remitted with intravenous adenosine. Despite treatment with sotalol, the crises became more frequent. An electrophysiological study was therefore ordered and was performed under general anesthetic. Given that there was no venous connection with the cardiac chambers, a 5-mm ablation catheter was introduced by a retroaortic approach (Therapy®, St. Jude Medical) into the left ventricle. Another 7-mm catheter (Celsius®, Biosense-Webster) was introduced through the esophagus to record atrial activity (Figs. 1A and B). The conduction intervals were normal. The anterograde and retrograde conductions were decremental. Tachycardia was easily induced with isoproterenol with both atrial and ventricular pacing, with a decrease in nodal conduction. The tachycardia was regular with a broad QRS interval and had the morphology of a complete right bundle branch block, with a cycle duration of 246ms, an atrial ratio of 1:1 and a ventriculoatrial interval of 24ms. The mapping catheter recorded His bundle activity 38ms prior to the ventriculogram (as at baseline). Atrial entrainment did not alter the QRS morphology. Ventricular entrainment occurred without fusion, with prolongation of the ventriculoatrial interval and ventricle-atrium-ventricle response, with a return cycle 116ms longer than the tachycardia cycle (Fig. 2). These data confirmed the nodal reentrant tachycardia with aberrant ventricular conduction. With the patient in sinus rhythm, the ablation catheter was guided to the region of the slow pathway, in the inferior part of the left atrial septum, as previously described.3 A less intense signal than the ventricular signal was observed (Figs. 1B and C). Junctional rhythm was produced mechanically. With left atrial pacing, a 35W radiofrequency pulse was applied at 55°C for 30s while atrioventricular conduction was monitored. Afterwards, tachycardia could not be induced and a nodal echo remained. No recurrences were found after 4 months of follow-up.
A: Anatomical schematic. B: Position of the ablation catheters. C: Electrogram at the application point. Abl, ablation catheter; Ao, aorta; Eso, esophagus; IVC, inferior vena cava; LAO, left anterior oblique; PA, pulmonary artery; RAO, right anterior oblique; SVC, superior vena cava.
In patients with tricuspid atresia who undergo Fontan palliation, supraventricular arrhythmias are usually atrial (atrial tachycardia and atrial fibrillation), with an incidence of up to 30%.2 Although the extracardiac cavopulmonary connection technique has reduced the incidence of these arrhythmias to less than 5%, by preventing dilatation and incisions in the right atrium, these substrates and other less common substrates (accessory pathway tachycardias and nodal tachycardias) still occur.2,3 The absence of venous approaches to the cardiac chambers hinders electrophysiological study and percutaneous catheter ablation. Alternative approaches have been described to treat atrial tachycardias, such as transthoracic puncture or direct puncture with the cannula used for the cavopulmonary shunt.4,5 Such procedures are complex and riskier than conventional approaches, particularly in children.
To our knowledge, there have been no reports of ablation of nodal tachycardia in patients who have undergone extracardiac Fontan palliation. The guided catheter introduced through the esophagus is easily manipulated and simplifies the study, as it can record activity and pace the left atrium. In addition, the retroaortic approach for the ablation catheter is easy and provides ready access to the lower part of the left atrial septum, which is the position of choice for ablation of nodal tachycardia in patients with tricuspid atresia.3 In these patients, the compact node usually lies next to the central fibrous body, underneath the atresic valve and above the ostium of the coronary sinus. A left septal approach is required to record the hisiogram and locate the fast pathway, as described by electroanatomic mapping.3 The slow pathway is located under this position, and ablation at this point can be safely and effectively performed.
.