Subcutaneous implantable cardioverter-defibrillators (S-ICD) are becoming established as an effective and safe therapy for a broad spectrum of patients.1,2 These devices do not require placement of endovascular leads in or around the heart and allow the sensing and appropriate treatment of malignant ventricular arrhythmias.3 Implantation is relatively simple, and the procedure times and results are very predictable. Nonetheless, physicians require a learning curve of about 13 implants in order to minimize potential complications.4 The implantation procedure recommended by the manufacturer involves 3 incisions (Figure A). A pocket incision on the lateral chest wall houses the pulse generator, and 2 parasternal incisions are made to position the defibrillation electrode: an inferior incision close to the xiphoid process and a superior incision to position the distal electrode parasternally at the level of the sternal angle.3 To minimize the risks associated with making 3 incisions, Knops et al5 developed a simplified implantation technique that omits the superior parasternal incision (Figure B). This incision is a frequent cause of discomfort, is difficult to suture, and is cosmetically unappealing to patients. In their series, Knops et al reported excellent results with this technique; however, their center has more experience with S-ICD implantation than any other in the world, and there are no other data in the literature. Here, we report our experience at a center with a less established track record with the 2-incision technique, used as first-line treatment in all patients from an early phase in the experience of the center.
Since October 2013, our team has implanted 17 S-ICDs in 17 patients, with follow-up for at least 1 month. For both the 3-incision and the 2-incision techniques, implantation was guided by anatomical landmarks, and fluoroscopy was not used in any procedure. The first 5 implantations were performed with the 3-incision technique. Subsequently, the 2-incision technique was selected as the first-line approach, with the option to revert to the 3-incision technique if difficulties were encountered in achieving a satisfactory implant. For the 2-incision technique, the insertion tool supplied with the S-ICD system was used in combination with an 11 Fr peel-away sheath of the type commonly used for transvenous lead placement.3 After the device-pocket and xyphoid incisions were made, the sheath was mounted over the insertion tool and the combined structure was tunneled parasternally. The insertion tool was then removed, leaving the peel-away sheath in place, and the electrode was introduced into the sheath. Once the electrode tip emerged subcutaneously from the sheath opening, it was held in place manually to prevent downward displacement, and the sheath was peeled away, leaving the distal sensing electrode in the desired position.5 The proximal sensing electrode was then secured at the paraxyphoid level, the pulse generator was connected, and both incisions were closed. The 2-incision technique was performed satisfactorily in all 12 patients in whom it was attempted, with no need for reversion to the 3-incision technique. General patient characteristics are shown in the Table. A ventricular fibrillation induction test was performed, and sustained arrhythmia was induced in 11 patients. Of these patients, 10 were adequately defibrillated with a single 65 J shock, and 1 patient required a second 65 J shock with reversed polarity. The mean treatment time for the 11 episodes of induced ventricular fibrillation was 16.6±3.4 s, and the mean effective-shock impedance was 81.5±13.6 Ω. Mean total procedure time (58.25±17.5 min) was notably shorter than for the 5 patients who underwent the 3-incision procedure (107.8±31 min); however, this difference may reflect not only the relative simplicity of the 2-incision method, but also the accumulated overall experience with the procedure. In all 12 patients, the device was programmed with 2 antitachycardia zones: 1 conditional discrimination zone and 1 shock zone. Patients were discharged the day after the procedure. After a mean follow-up of 6.25 months (range, 1-13 months), there have been no major or minor complications, no cases of lead displacement, and no need for reoperation. During follow-up, there have been no recorded events due to appropriate or inappropriate sensing and no inappropriate or appropriate shocks; these results are identical to those obtained in the patients who underwent implantation using the 3-incision method. Notably, the devices fitted in 6 of the patients who underwent the 2-incision procedure were programmed with the secondary sensing vector (between the distal electrode and the pulse generator), with no effect on the results; this sensing vector involves the distal sensing electrode, potentially the more vulnerable to problems due to lead dislocation in the 2-incision technique.
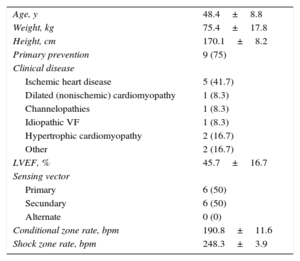
Characteristics of Patients
| Age, y | 48.4±8.8 |
| Weight, kg | 75.4±17.8 |
| Height, cm | 170.1±8.2 |
| Primary prevention | 9 (75) |
| Clinical disease | |
| Ischemic heart disease | 5 (41.7) |
| Dilated (nonischemic) cardiomyopathy | 1 (8.3) |
| Channelopathies | 1 (8.3) |
| Idiopathic VF | 1 (8.3) |
| Hypertrophic cardiomyopathy | 2 (16.7) |
| Other | 2 (16.7) |
| LVEF, % | 45.7±16.7 |
| Sensing vector | |
| Primary | 6 (50) |
| Secundary | 6 (50) |
| Alternate | 0 (0) |
| Conditional zone rate, bpm | 190.8±11.6 |
| Shock zone rate, bpm | 248.3±3.9 |
LVEF, left ventricular ejection fraction; VF, ventricular fibrillation.
Data are expressed as no. (%) or mean±standard deviation.
The results of our series show that the S-ICD can be appropriately positioned using the 2-incision technique, permitting cardiac signal detection without oversensing or undersensing, providing appropriate defibrillation, and ensuring system stability during follow-up. These results support the adoption of this technique as a first-line approach in S-ICD implantation.
CONFLICTS OF INTERESTM.A. Arias is a proctor for the S-ICD system and Associate Editor of Revista Española de Cardiología.