Infectious endocarditis (IE) still carries high morbidity and mortality. Currently, transesophageal echocardiography (TEE) is the reference imaging technique for the diagnosis and assessment of IE and its complications, but a series of noteworthy results have been published with multidetector computed tomography (MDCT) for presurgical assessment of IE.1–3 The new European Guidelines4 reinforce the role of MDCT both in suspected IE and in confirmed cases for assessment of complications with an extension of the major diagnostic criteria to include paravalvular lesions in MDCT. The European Society of Cardiology5 recommends preoperative assessment of coronary artery disease prior to surgery in selected patients; however, in the context of IE, invasive coronary angiography is associated with a nonnegligible risk of embolism.
We conducted a prospective study with the objective of assessing the utility of MDCT in IE. The study included 27 consecutive patients who met the diagnostic criteria for possible IE (41%) or definite IE (59%) according to the modified Duke criteria.4 A 64-detector device (thickness/cut increment 0.6/0.3mm, electrocardiogram-gated, field of view extended to the upper abdomen) was used with 80mL of intravenous contrast (350mg/mL, 5.5mL/s).
The results were compared with the findings from TEE and surgery in patients who underwent an intervention (Table). Five of the patients (18.5%) had device-associated IE (3 lead-associated and 2 central-catheter–associated) and 22 had valve-associated disease (57% associated with the native valve, 29% with a bioprosthesis, and 14% with mechanical valves).
Clinical Characteristics, Type of Endocarditis, Presence of Vegetation, Complications, and Coronary Anatomy
| Patient | Sex, age, y | Probability of IE | Heart disease/underlying condition | Vegetation observed in TEE | Vegetation observed in MDCT | Complication diagnosed in TEE | Complication diagnosed in MDCT | Coronary arteries in MDCT | Extracardiac findings in MDCT |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F, 74 | Possible | Mechanical mitral and aortic valve prostheses | No | No | Periaortic abscess Suspected fistula | Pseudoaneurysm Fistula ruled out | No lesions | Mycotic aneurysm in superior mesenteric artery |
| 2 | M, 81 | Possible | No | No | No | No | No | Two-vessel disease | Mural thrombus in ascending aorta |
| 3 | M, 62 | Definite | No | Yes (native aortic) | No | No | No | Unassessable Intense calcification | Embolization in spleen and psoas |
| 4 | M, 76 | Definite | Biological aortic valve prosthesis+ACBS | Yes (aortic biological) | Yes | MAJ abscess | No | Single-vessel disease Patent bypass | |
| 5 | M, 41 | Definite | No Intravenous drug user | Yes (native tricuspid) | No | No | No | No lesions | Pulmonary infarction |
| 6 | F, 82 | Possible | Biological aortic valve prosthesis+ACBS | Yes (native mitral) | No | No | No | Unassessable Intense calcification | |
| 7 | M, 65 | Definite | ACBS | Yes (native aortic) | Yes | No | Perforated leaflet | Three-vessel disease Patent bypass | Bilateral pleural effusion |
| 8 | M, 59 | Definite | Mechanical aortic valve prosthesis | Yes (mechanical aortic) | No | No | No | No lesions | Pleural effusion |
| 9 | F, 80 | Possible | ICD-CRT | Yes (lead) | No | No | No | Unassessable Intense calcification | |
| 10 | M, 30 | Possible | ICD | Yes (lead) | Yes | No | No | No lesions | |
| 11 | F, 66 | Definite | Mechanical aortic valve prosthesis and pacemaker | Yes (lead) | No | No | No | No lesions | |
| 12 | M, 68 | Definite | No | Yes (native mitral and aortic) | Yes | Perforated aortic leaflet Mitral chord rupture | Mitral chord rupture | No lesions | Splenic infarction Pleural effusion |
| 13 | M, 48 | Possible | Aortic prosthetic tube | No | No | No | Assessment aortic tube | No synchronization | Periaortic hematoma |
| 14 | F, 51 | Possible | Central catheter | Yes (catheter) | Yes | No | No | Not assessable due to contrast failure | Subclavian vein thrombosis |
| 15 | M, 84 | Possible | Central catheter | Yes (catheter) | No | No | No | Three-vessel disease | Pulmonary consolidation Jugular thrombosis |
| 16 | M, 60 | Definite | No | Yes (native mitral) | Yes | No | No | Right coronary and circumflex artery not assessable | Splenic infarction |
| 17 | F, 57 | Definite | Obstructive hypertrophic cardiomyopathy | Yes (native mitral) | Yes | MAJ abscess | MAJ abscess | No lesions | |
| 18 | M, 70 | Definite | Biological aortic valve prosthesis | Yes (aortic biological and native mitral) | Yes | MAJ abscess Prosthesis removal | MAJ abscess Prosthesis removal | No lesions | Aneurysm of ascending aorta Pleural effusion |
| 19 | M, 76 | Definite | Biological aortic valve prosthesis+ACBS | Yes (biological aortic) | Yes | MAJ abscess | MAJ abscess | LMCA disease+3 vessels Patent bypass | Splenic infarction Pleural effusion |
| 20 | F, 79 | Definite | Biological aortic valve prosthesis | Yes (MAJ) | Yes | MAJ abscess | MAJ abscess | No lesions | |
| 21 | M, 32 | Definite | Subaortic ventricular septal defect | Yes (native aortic) | Yes | No | No | No lesions | Splenic infarction |
| 22 | M, 60 | Definite | No | Yes (native mitral) | No | MAJ thickening | No | No lesions | Splenic infarction |
| 23 | F, 23 | Definite | Tetralogy of Fallot. Right ventricle to pulmonary artery conduit | Yes (biological pulmonary) | Yes | No | No | No lesions Assessment right ventricle-pulmonary artery conduit | Pulmonary thromboembolism |
| 24 | M, 39 | Possible | Bicuspid aortic valve | Yes (native aortic) | Yes | No | No | No lesions | Paraseptal emphysema |
| 25 | M, 78 | Definite | Biological aortic valve prosthesis | Yes (native mitral) | Yes | No | No | No lesions | Pleural effusion |
| 26 | M, 81 | Definite | Biological aortic valve prosthesis | No | No | Periaortic abscess | Periaortic abscess that infiltrates MAJ and encompasses LMCA, LADA, and CxA | LADA not assessable due to calcification Remaining arteries without lesions | Splenic infarction Pleural effusion |
| 27 | M, 59 | Definite | Mechanical aortic valve prosthesis | Yes (aortic root) | Yes | Periaortic abscess | Pseudoaneurysm in the sinus of Valsalva | No lesions |
ACBS, aortocoronary bypass surgery; CRT, cardiac resynchronization therapy; CxA, circumflex artery; ICD, implantable cardioverter device; IE, infectious endocarditis; F, female; LADA, left anterior descending artery; LMCA, left main coronary artery; M, male; MAJ, mitral-aortic junction; MDCT, multidetector computed tomography; TEE, transesophageal echocardiography.
Of note among the MDCT findings was the following:
- -
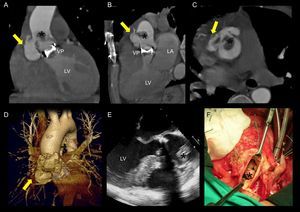
Suspected aortic fistula to the pulmonary trunk was ruled out and 2 suspected periaortic abscesses were appropriately assessed. These turned out to be pseudoaneurysms (Figure), in all cases associated with mechanical aortic valve prosthesis.
Figure.Mechanical aortic-valve-prosthesis–associated endocarditis with pseudoaneurysm of the aortic root. Multidetector computed tomography identified a pseudoaneurysm in the right sinus of Valsalva (yellow arrow) in the coronal (A), sagittal (B), and axial (C) plane, and in the 3-dimensional reconstruction (D), along with a large vegetation affixed to the proximal ascending aorta (*). The vegetation was observed in transesophageal echocardiography (E), but the pseudoaneurysm was not detected. These findings were confirmed during surgery (F). LA, left atrium; LV, left ventricle; VP, mechanical aortic valve prosthesis.
(0.42MB). - -
Supracoronary prosthetic graft was assessed and a large hematoma was appropriately characterized in the graft region, without leaks or endocardial complications; a graft from the right ventricle to the pulmonary artery was assessed, with exact determination of the diameter of the ascending aorta in a patient who finally required implantation of a valve tube.
- -
Four of the 6 abscesses of the mitral-aortic junction were diagnosed with TEE and confirmed by surgery. One of these abscesses, which was an extensive lesion, could not be evaluated by echocardiography. Tomography was able to adequately define the limits of the abscess, which extended to the aortopulmonary window and which encompassed the coronary artery origin.
- -
In 77% of the patients, the native coronary arteries or the bypass were assessed.
- -
In all patients who had undergone a repeat procedure, the distance from the apex of the right ventricle or bypass to the sternum was determined.
- -
In 70% of the patients, extracardiac findings were reported. This is particularly important as these are minor criteria for peripheral arterial embolic events (26%), pulmonary infarction (7.4%), and mycotic aneurysms (3.7%).
- -
Of the 17 vegetations detected in TEE, 12 were valve-associated (both native and prosthetic) in the MDCT and an additional 3 device-associated vegetations were detected. The thread-like and hypermobile vegetations were those not detected.
The use of MDCT in IE, reinforced in the new guidelines,4 has not yet been assessed in Spain. In the present study, based on an extensive series, we would highlight several conclusions:
- -
In valvular IE, MDCT is key for visualizing the aortic wall, which is usually incompletely assessed with echocardiography. This structure is often affected by fistulas, pseudoaneurysms, and abscesses. The greatest advantage is apparent in IE associated with mechanical aortic valve prosthesis, in which complications are frequently present. Assessment with TEE can be particularly complicated given the presence of acoustic shadows.
- -
In addition, the technique allows assessment of the coronary artery and estimation of the distance from the right ventricular apex or coronary bypass to the sternum in patients with prior surgery and is also useful in right-sided IE for diagnosis of pulmonary embolism.
- -
However, in our experience, the information provided by MDCT is less relevant both for assessment of vegetations (mainly thread-like ones) and for device-associated IE, given that in the latter case, local complications are not usually present and major surgery is not required, and so assessment of coronary anatomy is not necessary.
Currently, with the development of a range of different imaging modalities, it is the responsibility of the cardiologist to be aware of the advantages of each technique to achieve the highest diagnostic accuracy. We believe that MDCT undoubtedly complements TEE in the management of IE.