Valve surgery is the treatment of choice for mitral regurgitation (MR) when the latter is accompanied by ventricular dysfunction or its symptoms. In such cases, valve repair is usually preferred to valve replacement, since the prognosis is generally more favorable. However, despite the implementation of modern valve repair techniques, the rate of MR recurrence can come close to 30%1 and, in the case of ischemic MR, can reach nearly 50% at 2 years. This leads to a significant number of repeat valve interventions,2 which may involve a high degree of risk, especially in elderly patients or those with numerous comorbidities.
The MitraClip device (Abbott Laboratories, Abbott Park, Illinois, United States) has been shown to be a safe and effective therapy that improves the symptoms of patients who are unable to undergo surgery.3 The experience gained in recent years has allowed the indications for this treatment to be extended to other groups of patients with MR. The treatment of patients with a prior failed annuloplasty has been reported previously,4 but the information concerning this scenario is still limited. The objective of this study was to present the experience in the treatment of failed annuloplasties with MitraClip in Spain. Between October 2010 and October 2015, 300 MitraClip implantations were performed in the Iberian Peninsula; they include a subseries of 8 procedures (2.6%) performed in 6 patients, which were carried out in annuloplasty rings.
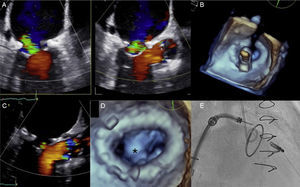
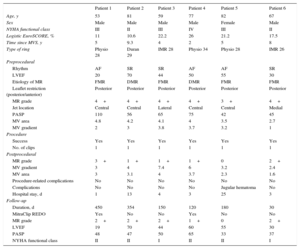
The characteristics of the population, the procedure, and follow-up are shown in the Table. The median time between annuloplasty and MitraClip implantation was 5 years, and the most common cause was recurrence in patients treated surgically for functional MR. In most cases, a central regurgitant jet was encountered, although, in 2 patients, the jet was proximal to the commissures. The procedure was successful in all the patients, resulting in a significant reduction of MR (Figures A-E), although when monitored prior to discharge, patient no. 1 was found to have grade 3+MR (the acute result according to transesophageal echocardiography performed at the end of the procedure was grade 2+MR, thus indicating a successful intervention). There were no major complications and the median hospital stay was 3.5 days. Recurrence of MR was detected during follow-up in 2 patients. In both, the procedure could be repeated to place a new clip, which resulted in trivial MR, without drastic reductions in valve area or excessive increases in the gradient. Patient no. 1 remained in good clinical condition until 9 months after the procedure. At that time, he was in a higher functional class and imaging studies revealed MR progression due to an increase in the width of the jet medial to the implanted clip (in connection with the severe restriction of the posterior leaflet). The options were studied and the decision was made to implant a new device in the central jet, which resulted in a sustained reduction of MR to grade 2+and, again, an improvement in the functional class. After the initial success, follow-up of patient no. 4 revealed MR recurrence lateral to the implanted clip, which was treated with another device 6 months later. At the time of writing, after a median follow-up of 165 days, all the patients were alive, were in New York Heart Association class ≤ II, and had MR ≤ 2+with gradients similar to those observed after the initial procedure. Only patient no. 3 had a noteworthy increase in the gradient, with no clinical impact, in connection with the annulus area according to planimetric measurement (2.4cm2); this measurement was 4cm2 at the level of the mitral orifice. Moreover, a reduction of the pulmonary pressure from 60.5mmHg to 47.5mmHg was observed.
Patient Characteristics at Baseline, According to Echocardiography, and During the Procedure and Follow-up
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | |
|---|---|---|---|---|---|---|
| Age, y | 53 | 81 | 59 | 77 | 82 | 67 |
| Sex | Male | Male | Male | Male | Female | Male |
| NYHA functional class | III | II | III | IV | III | II |
| Logistic EuroSCORE, % | 11 | 10.6 | 22.2 | 26 | 21.2 | 17.5 |
| Time since MVS, y | 5 | 9.3 | 4 | 2 | 5 | 8 |
| Type of ring | Physio 28 | Duran 29 | IMR 28 | Physio 34 | Physio 28 | IMR 26 |
| Preprocedural | ||||||
| Rhythm | AF | SR | SR | AF | AF | SR |
| LVEF | 20 | 70 | 44 | 50 | 55 | 30 |
| Etiology of MR | FMR | DMR | FMR | DMR | FMR | FMR |
| Leaflet restriction (posterior/anterior) | Posterior | Posterior | Posterior | Posterior | Posterior | Posterior |
| MR grade | 4+ | 4+ | 4+ | 4+ | 3+ | 4+ |
| Jet location | Central | Central | Lateral | Central | Central | Medial |
| PASP | 110 | 56 | 65 | 75 | 42 | 45 |
| MV area | 4.8 | 4.2 | 4.1 | 4 | 3.5 | 2.7 |
| MV gradient | 2 | 3 | 3.8 | 3.7 | 3.2 | 1 |
| Procedure | ||||||
| Success | Yes | Yes | Yes | Yes | Yes | Yes |
| No. of clips | 1 | 1 | 1 | 1 | 1 | 1 |
| Postprocedural | ||||||
| MR grade | 3+ | 1+ | 1+ | 1+ | 0 | 2+ |
| MV gradient | 3 | 4 | 7.4 | 6 | 3.2 | 2.4 |
| MV area | 3 | 3.1 | 4 | 3.7 | 2.3 | 1.6 |
| Procedure-related complications | No | No | No | No | No | No |
| Complications | No | No | No | No | Jugular hematoma | No |
| Hospital stay, d | 1 | 13 | 4 | 3 | 25 | 3 |
| Follow-up | ||||||
| Duration, d | 450 | 354 | 150 | 120 | 180 | 30 |
| MitraClip REDO | Yes | No | No | Yes | No | No |
| MR grade | 2+ | 2+ | 2+ | 1+ | 0 | 2+ |
| LVEF | 19 | 70 | 44 | 60 | 55 | 30 |
| PASP | 48 | 47 | 50 | 65 | 33 | 37 |
| NYHA functional class | II | II | I | II | II | I |
AF, atrial fibrillation; DMR, degenerative mitral regurgitation; FMR, functional mitral regurgitation; LVEF, left ventricular ejection fraction; MR, mitral regurgitation; MV, mitral valve; MVS, mitral valve surgery; NYHA, New York Heart Association; PASP, pulmonary artery systolic pressure; SR, sinus rhythm.
A: Severe mitral regurgitation following annuloplasty; B: Real-time 3-dimensional transesophageal echocardiogram showing perpendicularity of the clip with respect to leaflets and ring; C: Achievement of mild mitral regurgitation following clip implantation; D: 3-dimensional transesophageal echocardiogram showing a double orifice with the clip in between (asterisk); E: Fluoroscopic image showing the position of the implanted clip in relation to the annuloplasty ring.
In this series, the largest reported in literature, we describe our experience in the treatment of MR following annuloplasty. The data show that the procedure is safe and that a satisfactory outcome is usually achieved with a single clip. However, in the case of recurrence, our results demonstrate that a second clip can be implanted without significantly affecting the mitral valve area or the resulting gradient. This finding is of great importance as it is the first time that it has been reported in the literature, and because the possibility of inducing mitral stenosis is a cause for concern when the MitraClip is used in this scenario (due to the reduction of the area caused by the ring). The main determinants for the use of the device are the presence of leaflets of adequate length, a clear view of these leaflets (sometimes shadowed by the effect of the ring itself) and, given that a marked restriction of the posterior valve is usually encountered, the freedom to maneuver the device to ensure access to the site where MR is most severe. In this respect, wide experience with the use of the MitraClip is essential.
The possibility of drawing conclusions from our study is limited in terms of the predictors of recurrence; however, in both of our cases of MR recurrence, the marked restriction of the posterior leaflet played a relevant role. In patients with extreme restriction of this leaflet (immobile posterior leaflet), perhaps other therapeutic alternatives should be considered.
In short, the MitraClip is a safe and effective option for the treatment of MR following surgical annuloplasty.
CONFLICTS OF INTERESTR. Estévez-Loureiro, D. Arzamendi, F. Carrasco-Chinchilla, and X. Freixa are proctors for MitraClip and have received conference fees from Abbot Vascular. J. Suárez de Lezo has also received conference fees from Abbot Vascular.