Cerebrovascular diseases are the second leading cause of death in Spain, and extracranial carotid disease is responsible for one-third of ischemic strokes. The indication for revascularization of a carotid lesion will be determined by the patient's symptomatic status and the severity of obstruction. Endovascular intervention with a stent is an optimal form of carotid revascularization, and the medium- and long-term results are similar to those of endarterectomy.1
Interventional cardiologists have proved to be professionals with optimal skills for safely deploying the stent in the carotid artery.2 However, in contrast to the situation outside Spain, interventional cardiologists do not participate in this type of procedure in this country.3
The Endovascular Unit of the Hospital Virgen Macarena in Seville, Spain, combines endovascular care with care of cardiovascular diseases. The unit is a multidisciplinary group for the treatment of carotid disease and is composed of interventional cardiologists and neurologists. The integrative approach represents an innovation in Spain.
The role of the neurologist consists of indicating the procedure, performing the clinical monitoring during the intervention, and conducting the follow-up. Interventional cardiologists have participated in a dedicated training program for carotid revascularization with stents, under the initial tutelage of an interventional radiologist. In addition, the cardiologists were trained by an interventional neuroradiologist in the handling of the devices to enable resolution of intracranial thromboembolic complications.
This letter presents our experience of stent revascularization of extracranial carotid lesions, and assesses whether the skills of interventional cardiologists can be readily transferred to this procedure to reduce the steepness of the learning curve.
From May 2008 through April 2014, 300 patients with carotid lesions were revascularized. These patients, with a mean (standard deviation [SD]) age of 68.9 (8.6) years, were mainly symptomatic (81.3%). Overall, 53% of the patients were diagnosed with a lesion in another vascular territory, mainly in the lower limbs (31%) and coronary arteries (23.7%).
Access was mainly transfemoral (91%), although in the last 2 years, right transradial access has started to be used for ipsilateral carotid interventions. The rate of aortic arches not readily amenable to carotid catheterization was 26%. Significant disease (< 50%) of the contralateral carotid artery was found in 48% of the patients.
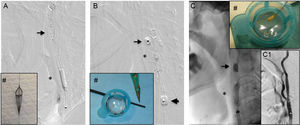
In all interventions, the use of brain protection devices was considered, although this was not feasible in 11 (4%). Distal protection was used in two-thirds of the patients. In most cases, a filter-type device was used (56%), although distal balloon occlusion was also used (11%). Proximal protection was used in 75 procedures (29%). In general, in the case of hypoechogenic or anechogenic plaques with a high degree of obstruction, proximal protection and, more recently, an occluding balloon was chosen as distal protection (Figure).
Embolic material extracted (#) after carotid stent dilation (*) in procedures using different methods of brain protection. A: Distal protection with protection device deployed in distal cervical carotid artery (unshaded arrow). B: Proximal protection with occlusion of blood flow through balloon inflation in exterior carotid artery (unshaded arrow) and common carotid artery (shaded arrow). C: Distal protection with occluder balloon in intrastentregion of the interior carotid artery. C1: Final outcome.
The overall success rate, taken as revascularization with residual stenosis < 50% and absence of major events (death, stroke, or infarction) in the first 24hours, was 98%. A major clinical event occurred in 6 patients (1 major stroke, 4 minor strokes, and 1 non-ST-elevation myocardial infarction).
Once the periprocedural phase had passed and during the first 30 days, 4 patients died (3 due to intracranial hemorrhage probably caused by hyperperfusion syndrome, and 1 due to thrombosis probably arising from the stent), and 4 had a stroke. Thus, overall, the composite rate of neurological events (death or stroke) at 30 days was 4.3%. These clinical outcomes were similar to those obtained in other Spanish studies4 (Table).
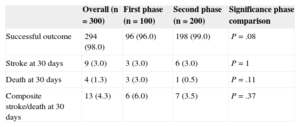
Overall Clinical Outcomes by Phase of Experience
| Overall (n = 300) | First phase (n = 100) | Second phase (n = 200) | Significance phase comparison | |
|---|---|---|---|---|
| Successful outcome | 294 (98.0) | 96 (96.0) | 198 (99.0) | P = .08 |
| Stroke at 30 days | 9 (3.0) | 3 (3.0) | 6 (3.0) | P = 1 |
| Death at 30 days | 4 (1.3) | 3 (3.0) | 1 (0.5) | P = .11 |
| Composite stroke/death at 30 days | 13 (4.3) | 6 (6.0) | 7 (3.5) | P = .37 |
Data expressed as No. (%).
To assess the impact of our learning curve, we compared the clinical outcomes obtained in the first third of our experience (100 initial procedures) with the remaining 200 interventions. The success rate was very high from the start of the program (96%), although there was a tendency toward a higher success rate during the period with greatest cumulative experience (99%; P = .08). No significant differences were found between periods in the composite events in the first 30 days, but the outcomes were better in the final phase of our experience (3.5% vs 6.0% initially; P = .37) due to a lower mortality rate (0.5% vs 3% initially; P = .11). These outcomes indicate that, although a learning curve for the intervention does exist, the interventional cardiologists showed an appropriate skills transfer right from the outset (Table).
In conclusion, our multidisciplinary model for the endovascular treatment of carotid disease showed optimal clinical outcomes, within the limits of excellence recommended by clinical practice guidelines,5 in a high-risk population (mainly symptomatic, elderly, and with a high atherosclerotic burden).