Patent ductus arteriosus is frequent in premature babies. With an incidence of 1:2500-5000, it accounts for 9% to 12% of congenital heart disease.1 Several different drugs have been tried for closure of hemodynamically significant patent ductus arteriosus. The first to be used was indomethacin, with a success rate of 70% and a reopening rate of 35%; however, the high cost of this drug has driven the search for other options such as ibuprofen.2 But such drugs are not harmless and are associated with decreased renal, mesenterial, and cerebral perfusion, and ibuprofen is associated with hyperbilirrubinemia.3 Recently, paracetamol has been demonstrated to be effective in this indication, with no reports of toxicity to date.
In this study, we report the use of oral paracetamol in premature babies. The drug was safe and effective at closing the hemodynamically significant patent ductus arteriosus. Premature patients in their first 10 days of life with a gestational age of 30 to 36 weeks and hemodynamically significant patent ductus arteriosus were included in this study. The defect was considered hemodynamically significant when the Qp/Qs ratio was greater than 1.5/1 and the left atrium/aortic root ratio was greater than 1.8 in echocardiography and the patient needed ventilatory support.2 Patients with heart disease resulting from the defect, intraventricular hemorrhage, thrombocytopenia, renal failure, hyperbilirubinemia, and necrotizing enterocolitis were excluded. Patients were divided into 2 groups according to weight: group 1 weighing less than 1kg and group 2 weighing more than 1kg. Both groups were treated with oral paracetamol at 15mg/kg/dose every 6hours (total cumulative dose 60mg/kg). Echocardiographic follow-up was done at 48hours after the first dose. A second cycle of the drug was administered if the ductus arteriosus had not closed. If the ductus arteriosus still had not closed after this second cycle, the patient was referred for surgical closure. All patients received fluid therapy on the first day at 70mL/kg/d, with a daily increase of 10 to 20mL/kg/d up to a maximum of 160mL/kg/d at the end of the first week of life.
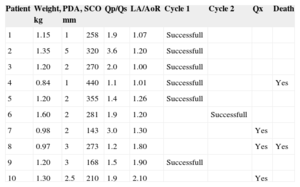
Ten patients were included for pharmacological treatment. Of these, closure was obtained in 6 with the first cycle of treatment. Four patients entered a second cycle, with 1 additional closure reported. The remaining 3 patients underwent surgery, with a final success rate of 70%. The success rate was greater in patients weighing more than 1kg (6 patients). There ratio of girls to boys was 3/1 (75%). As shown in Table, the size of the ductus arteriosus ranged from 1mm to 5mm in diameter. The echocardiographic parameters were as follows: mean cardiac load in systole 292.5mmHg (range, 143-440mmHg), mean Qp/Qs ratio 2 (range, 1.1-3.5), mean left atrium/aortic root ratio 1.23 (range, 1-1.8). Liver function and platelet count were monitored during treatment, with no significant changes observed.
Characteristics of Patients Included in the Study
| Patient | Weight, kg | PDA, mm | SCO | Qp/Qs | LA/AoR | Cycle 1 | Cycle 2 | Qx | Death |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 1.15 | 1 | 258 | 1.9 | 1.07 | Successfull | |||
| 2 | 1.35 | 5 | 320 | 3.6 | 1.20 | Successfull | |||
| 3 | 1.20 | 2 | 270 | 2.0 | 1.00 | Successfull | |||
| 4 | 0.84 | 1 | 440 | 1.1 | 1.01 | Successfull | Yes | ||
| 5 | 1.20 | 2 | 355 | 1.4 | 1.26 | Successfull | |||
| 6 | 1.60 | 2 | 281 | 1.9 | 1.20 | Successfull | |||
| 7 | 0.98 | 2 | 143 | 3.0 | 1.30 | Yes | |||
| 8 | 0.97 | 3 | 273 | 1.2 | 1.80 | Yes | Yes | ||
| 9 | 1.20 | 3 | 168 | 1.5 | 1.90 | Successfull | |||
| 10 | 1.30 | 2.5 | 210 | 1.9 | 2.10 | Yes |
AoR, aortic root; LA, left atrium; PDA, patent ductus arteriosus; SCO, systolic cardiac output.
Two patients died: patient 4 due to septic shock, with death occurring 48hours after completing the treatment cycle and patient 8 due to hypovolemic shock after surgery (Table). These deaths were not considered related to drug administration.
The success rate for closure of the ductus arteriosus with paracetamol is similar to that of nonsteroidal antiinflammatory drugs, which also have a success rate of 70%. As in this study, other authors have found that paracetamol has similar success rates to other drugs. For example, the Cochrane Plus review in 2008 found a success rate for indomethacin of approximately 70%.2 In another study by Jones et al,4 indomethacin was compared to ibuprofen in the treatment of hemodynamically significant patent ductus arteriosus in premature patients. The authors found that indomethacin was effecive in up to 70% of cases in the first cycle and in 60% when a second cycle was required. With ibuprofen, the closure rate was 75% in the first cycle and 55% in the second cycle. In the study conducted by Ozmert et al,5 a success rate of 71.4% was reported with the use of paracetamol. These success rates are similar to those found in the present series. It is important to highlight paracetamol is apparently innocuous: no short- or medium-term complications were reported. This is presumably because the drug works through nonselective inhibition of cyclooxygenase, the enzyme responsible for prostaglandin synthesis, without any vasoconstriction or reduction in renal, mesenterial, or cerebral blood flow.6 Paracetamol is readily available and innocuous in neonates. Its ability to induce closure of hemodynamically significant patent ductus arteriosus may therefore shorten intrahospital stays and reduce associated morbidity.
Limitations of this study include the small number of patients, which means that precise conclusions cannot be drawn. Nevertheless, so far paracetamol has been shown to be effective with few side effects. Larger studies with longer follow-up would be needed to more clearly demonstrate the pharmacological effect and provide a more rigorous analysis of potential complications.