Circulatory support devices such as veno-arterial extracorporeal membrane oxygenation (VA-ECMO) help maintain hemodynamic support and adequate tissue oxygenation, and form part of the therapeutic armamentarium in cardiac arrest and refractory cardiogenic shock.1–3 Percutaneous implantation is less invasive than the approach used in other short-term devices, with femoral cannulation most commonly used due to its simplicity and speed.4 VA-ECMO can be used as a bridge to recovery or to the decision for a long-term ventricular assist device or heart transplantation. It is in widespread use,3 and experience continues to increase in adult patients in Spain,5 where the sole alternative is cardiac surgery.
It is well known that early treatment with appropriate circulatory support is vital in patients with cardiogenic shock.1–3 For this reason, in July 2013 we set up a transfemoral percutaneous ECMO implantation program in nonsurgical patients with refractory cardiogenic shock at our hospital. The interventional cardiologist implanted the CARDIOHELPTM system (MAQUET Cardiopulmonary AG, Germany) in all patients in the cardiac catheterization laboratory, and inpatient care then continued in the cardiac intensive care unit. This article describes the baseline patient characteristics; the indications, duration and management of circulatory support; and progress at follow up.
Between July 2013 and April 2014 VA-ECMO was implanted in 4 consecutive patients with refractory cardiogenic shock, INTERMACS level 1 (critical cardiogenic shock).6 Three of these patients had cardiogenic shock following an anterior, inferior and right ventricular myocardial infarction, respectively, and the fourth had a refractory cardiac arrest secondary to an anterior infarction. The baseline characteristics and the clinical progress of the 4 patients are described in the Table. The mean (standard deviation) age was 54.5 (7.4) years. Three patients were male. The mean left ventricular ejection fraction before ECMO implantation was 10% (5%) (n=3) and the fourth patient had severe right ventricular dysfunction. The decision to implant VA-ECMO was made in the cardiac catheterization laboratory due to poor clinical outcome of the primary percutaneous coronary intervention. An interventional cardiologist performed the cannulation. Implantation was successful in all cases and the mean time to pump initiation was 14 (8-20) minutes. At 24hours postcannulation, lactic acid levels had dropped from a precannulation baseline of 8.4 (1.7) mmol/L to 2.3 (1) mmol/L (P<.001). All patients had previously had intra-aortic balloon counterpulsation implantation via the contralateral femoral artery. Due to their clinical status, all patients required invasive mechanical ventilation, and a Swan-Ganz catheter for hemodynamic monitoring.
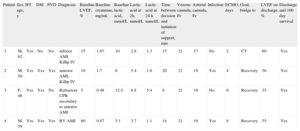
Baseline Characteristics and Progress of Patients With Veno-arterial Extracorporeal Membrane Oxygenation
| Patient | Sex, age, y | HT | DM | PVD | Diagnosis | Baseline LVEF, % | Baseline creatinine, mg/mL | Baseline lactic acid, mmol/L | Lactic acid at 2h, mmol/L | Lactic acid at 24 h mmol/L | Time between decision and initiation of support, min | Venous cannula, Fr | Arterial cannula, Fr | Infection | ECMO, days | Goal, bridge to | LVEF on discharge, % | Discharge and 100 day survival |
| 1 | M, 62 | Yes | No | No | inferior AMI, Killip IV | 15 | 1.67 | 10 | 2.8 | 1.3 | 15 | 21 | 17 | No | 2 | CT | 60 | Yes |
| 2 | M, 50 | Yes | Yes | Yes | anterior AMI, Killip IV | 10 | 1.7 | 6 | 5.4 | 1.6 | 20 | 21 | 19 | Yes | 4 | Recovery | 30 | Yes |
| 3 | F, 46 | Yes | Yes | No | Refractory CPR secondary to anterior AMI | 5 | 0.48 | 12.5 | 8.8 | 5.4 | 8 | 21 | 19 | No | 6 | Recovery | 35 | Yes |
| 4 | M, 59 | Yes | Yes | Yes | RV AMI | 60 | 0.87 | 5.1 | 3.7 | 1.1 | 14 | 21 | 19 | Yes | 8 | Recovery | 55 | Yes |
AMI, acute myocardial infarction; CPR, cardiopulmonary arrest; CT, cardiac transplantation; DM, diabetes mellitus; ECMO, extracorporeal membrane oxygenation; F, female; HT, hypertension; LVEF, left ventricular ejection fraction; M, male; PVD, peripheral vascular disease; RV, right ventricular.
Patient 1 had a successful heart transplantation, hence normal LVEF on discharge.
In all patients we achieved the initial goal of providing a bridge to heart transplantation (patient 1), and to recovery (patients 2, 3 and 4). The mean duration of support was 5 (2.5) days, and none of the patients had serious complications such as stroke or lower limb ischemia (in all patients angiography was performed prior to implantation to check that femoral artery size was adequate, and as a guide for cannula size). Two patients (1 and 4) required multiple blood product transfusions, specifically upon initiation of support, with subsequent stabilization, and 2 patients required intravenous antibiotic treatment for infectious complications (Table). We managed to wean 3 patients (75%) off the device, following revascularization and recovery of ventricular function. The other patient (patient 1) required implantation of a Berlin Heart EXCOR biventricular assist device as a bridge to heart transplantation, which was subsequently performed successfully. Survival to discharge and 100-day survival were both 100%. Left ventricular ejection fraction on discharge is shown in the Table.
Our study has the limitations of being single center and having a small sample number. However, our initial experience shows that early implantation of percutaneous VA-ECMO in the cardiac catheterization laboratory, carried out by an interventional cardiologist, in patients with refractory cardiogenic shock secondary to myocardial infarction, is feasible and safe, and avoids dependence on surgical treatment and possible delay in its performance in extreme clinical emergencies. Appropriate patient selection is fundamental, and VA-ECMO implantation probably has a stronger indication in patients with acute and potentially reversible heart failure, as a bridge to recovery, long-term circulatory assist device implantation, or heart transplantation.
FundingThis work was partially supported with Fondo de Desarrollo Regional (FEDER-UE)/Instituto de Salud Carlos III (ISCIII) and Red de Investigación Cardiovascular (RIC) RD12/0042.