In recent years, the use of invasive strategies has become the generalized approach in the management of patients with acute coronary syndrome, not only those with ST-segment elevation, but also in those with non–ST-segment elevation (NSTEACS). An invasive strategy is justified by the associated prognostic benefit due to reduced mortality.1,2 However, the benefits of an invasive approach in NSTEACS are not all that clear in certain subgroups in which the risks and consequences of percutaneous coronary intervention (PCI) can outweigh the benefit associated with revascularization.3 One of the groups in which the benefit of an invasive approach is not clear is the population with significant anemia. In these patients, aggressive antithrombotic therapy associated with an invasive approach can produce deleterious effects, exacerbate the severity of anemia and, consequently, decrease oxygen delivery to tissue with an already reduced oxygen supply. A number of studies have demonstrated the independent negative prognostic value of anemia in acute coronary syndrome, which has been proposed as a variable to be taken into account in mortality risk stratification in these patients.4,5 In this context, we describe our experience in the management of patients hospitalized for NSTEACS with hemoglobin levels < 10g/dL on admission.
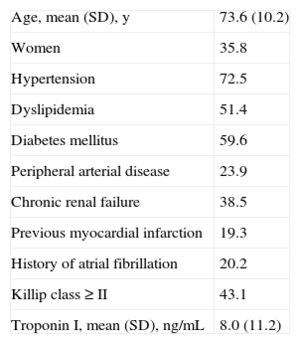
For this purpose, we used data from the CardioCHUS Registry, which includes 5443 acute coronary syndrome patients consecutively admitted to Hospital Clínico de Santiago in northwestern Spain (2003-2012); 3689 were admitted with NSTEACS, 765 of whom (20.7%) had anemia at admission (hemoglobin < 12g/dL in women and < 13g/dL in men); 109 (2.9%) had severe anemia, defined as hemoglobin levels < 10g/dL. The main baseline characteristics of these patients are summarized in the Table. In comparison with those without severe anemia, patients with hemoglobin < 10g/dL were older (mean age [standard deviation], 73.6 [SD,10.2] years vs 67.5 [SD,12.2] years; P=.001) and had a higher prevalence of diabetes mellitus (59.6% vs 29.2%; P<.001), hypertension (72.5% vs 60.3%; P=.010), and peripheral arterial disease (23.9% vs 10.3%; P<.001), poorer renal function (mean creatinine level, 1.8 [SD,1.1] mg/dL vs 1.1 [0.6] mg/dL; P<.001), and worse functional class (Killip ≥ 2, 43.1% vs 15.3%; P<.001). On admission, there was evidence of active bleeding in 33 patients (30.3%) (the origin was gastrointestinal in 23, urinary in 6, and respiratory in 4), and 58 patients required at least 1 transfusion.
Baseline Characteristics of the Patients Hospitalized With Non–ST-Segment Elevation Acute Coronary Syndrome and Hemoglobin Levels Less Than 10g/dL at Admission
| Age, mean (SD), y | 73.6 (10.2) |
| Women | 35.8 |
| Hypertension | 72.5 |
| Dyslipidemia | 51.4 |
| Diabetes mellitus | 59.6 |
| Peripheral arterial disease | 23.9 |
| Chronic renal failure | 38.5 |
| Previous myocardial infarction | 19.3 |
| History of atrial fibrillation | 20.2 |
| Killip class ≥ II | 43.1 |
| Troponin I, mean (SD), ng/mL | 8.0 (11.2) |
SD, standard deviation.
Data are expressed as no. (%) or mean (standard deviation).
Of the 109 patients with NSTEACS and hemoglobin < 10g/dL, 75 patients (68.8%) underwent cardiac catheterization. No significant differences were found between the patients who underwent an invasive strategy and those receiving conservative treatment (without catheterization) in terms of age, sex, the incidence of diabetes mellitus, hypertension, dyslipidemia, chronic renal failure, peripheral arterial disease, or mean hemoglobin level. Thirty-five patients underwent PCI, 32 with implantation of a conventional stent and 2 with a drug-eluting stent; only 1 patient underwent simple angioplasty. The management of the patients with severe anemia was most often conservative (without catheterization, 31.2% vs 21.0% of the patients with mild anemia vs 10.4% of those without anemia; P<.001), and PCI was less widely performed (32.1% vs 45.3% of the patients with mild anemia and vs 53.7% of the patients without anemia; P<.001).
Regarding drug therapy, on admission, 99 patients (90.8%) were prescribed acetylsalicylic acid, 70 (64.2%) clopidogrel, 57 (52.3%) beta-blockers, 50 (45.9%) angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers, and 79 (72.5%) statins. Low-molecular-weight heparin was used in 76 patients (69.7%), unfractionated heparin in 16 (14.7%), and fondaparinux in 12 (11.0%). Dual antiplatelet therapy was initiated on admission in 67 patients (61.5%), although only 34 (31.2%) continued taking 2 antiplatelet agents at discharge and 42 (38.5%) were taking 1. Twelve patients (11.0%) left the hospital with a prescription for oral anticoagulation therapy.
There were 13 in-hospital deaths (11.9%). Mortality was higher in patients with severe anemia than in those with mild anemia (8.4%) or without anemia (2.8%); 14 patients (12.8%) experienced heart failure during their hospital stay and another 14 (12.8%) had refractory angina. The performance of PCI had no significant impact on in-hospital mortality (odds ratio [OR]=0.40; 95% confidence interval [95%CI], 0.09-1.83; P=.239) or on the combination of death, heart failure, and refractory angina (OR=0.45; 95%CI, 0.29-1.75; P=.450).
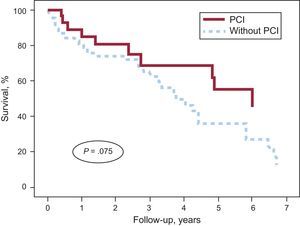
Of the 96 patients who were discharged from the hospital, half (n=48) died during follow-up (2.8 [2.5] years), 20 (20.8%) had a reinfarction, and 32 (33.3%) experienced heart failure. In the univariate analysis, the performance of PCI was associated with a lower mortality rate during follow-up (hazard ratio [HR]=0.49; 95%CI, 0.25-0.94; P=.032); however, this significance was lost after adjustment for the GRACE (Global Registry of Acute Coronary Events) score at hospital discharge, and a trend toward a lower mortality rate persisted (HR=0.52; 95%CI, 0.26-1.07; P=.075) (Figure).
Survival curves for patients with non-ST-segment elevation acute coronary syndrome and severe anemia (hemoglobin < 10g/dL) at admission, stratified according to whether or not they had undergone PCI, and after adjustment for the GRACE score at discharge. GRACE, Global Registry of Acute Coronary Events; PCI, percutaneous coronary intervention.
Thus, we conclude that, in routine clinical practice, it is not uncommon to encounter patients admitted for NSTEACS who have severe anemia (3 out of every 100), a comorbidity that will influence the treatment of the coronary event, and most patients are undertreated with respect to currently recommended drug therapy. The prognosis of these patients is frankly poor, with a mortality rate higher than 10% during the hospital stay and greater than 50% at 3 years. The interventional strategy has not been shown to reduce the high in-hospital mortality rate in this patient population, although there is a trend toward a reduction in long-term mortality.