Catheter ablation is the recommended treatment in patients with paroxysmal atrial fibrillation refractory to antiarrhythmic therapy or with symptomatic persistent atrial fibrillation that cannot be controlled by other therapeutic strategies.1 The main objective of this procedure is electrical isolation of the pulmonary veins.2 The most widely used techniques are point-by-point radiofrequency ablation and cryoablation.2 Recently, an ablation system has been introduced that uses laser energy. The catheter, which includes a compliant balloon, enables direct visualization of left atrium and the pulmonary veins to guide the ablation. The first clinical results showed good safety and efficacy.3–5 Our objective was to describe the first use of the laser balloon catheter for pulmonary vein isolation in Spain, evaluating its efficacy and safety.
We included patients who underwent ablation of atrial fibrillation between February 2013 and March 2014. All patients signed an informed consent form. We excluded those with a long history of persistent atrial fibrillation or significant structural heart disease.
The ablation system (CardioFocus, Marlborough, Massachusetts, United States) includes the following components (Figure A): a steerable sheath (15 Fr), adaptable to a balloon catheter, with an adjustable diameter (up to 35mm) and an atraumatic tip (Figure B); an endoscope (2 Fr); an optical fiber; and a console for selection of the power and duration of the applications. The endoscope and optical fiber are inserted via the balloon catheter. As viewed with the endoscope, blood is red and the tissue in contact with the balloon is white (Figure C); there is a blind area of 45°, making it necessary to rotate the catheter to complete the ablation line. Energy (a 980nm diode laser) is applied by the optical fiber.
A quadripolar catheter was used to stimulate the phrenic nerve during ablation and an esophageal temperature probe was inserted. Following pulmonary vein angiography, the balloon catheter was introduced and was inflated until the occlusion of each vein was completed. The antral or ostial anatomy was confirmed by the radiological or endoscopic image. The objective was to direct the laser beam as close as possible to the antrum. Each application overlapped the preceding one by 30% to 50% to achieve a continuous ablation line. The energy applied (5.5-12W) was adjusted according to the expanse of tissue visualized and the presence of blood trapped by the balloon. Once the circumference of each vein had been completely encircled, bidirectional block was confirmed. When conduction persisted, additional applications were carried out in accordance with Lasso® catheter recordings.
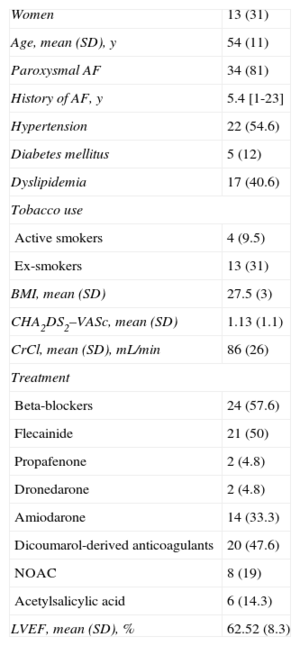
Forty-two patients underwent laser catheter ablation. The patients’ characteristics are summarized in the Table. The pulmonary vein anatomy was normal in 86% of the patients, that of the left common pulmonary vein in 7%, and that of the right common pulmonary vein in 5%. The mean duration (standard deviation) of the procedure was 159 (30) minutes, with a mean fluoroscopy time of 41 (15) minutes. In all, 162 (99%) of the 164 veins included were isolated. Ablation of both ipsilateral veins was accomplished with a single encirclement in 21% of the patients. Isolation of 89% of the pulmonary veins was achieved after completion of the first ablation line. The structure requiring the greatest number of applications was the left common pulmonary vein. Comparison of the procedure times of the first 6 and last 6 months revealed a reduction in fluoroscopy time (46minutes vs 36minutes; P=.05), but no change in the total procedure time.
Sample Characteristics (n=42)
| Women | 13 (31) |
| Age, mean (SD), y | 54 (11) |
| Paroxysmal AF | 34 (81) |
| History of AF, y | 5.4 [1-23] |
| Hypertension | 22 (54.6) |
| Diabetes mellitus | 5 (12) |
| Dyslipidemia | 17 (40.6) |
| Tobacco use | |
| Active smokers | 4 (9.5) |
| Ex-smokers | 13 (31) |
| BMI, mean (SD) | 27.5 (3) |
| CHA2DS2–VASc, mean (SD) | 1.13 (1.1) |
| CrCl, mean (SD), mL/min | 86 (26) |
| Treatment | |
| Beta-blockers | 24 (57.6) |
| Flecainide | 21 (50) |
| Propafenone | 2 (4.8) |
| Dronedarone | 2 (4.8) |
| Amiodarone | 14 (33.3) |
| Dicoumarol-derived anticoagulants | 20 (47.6) |
| NOAC | 8 (19) |
| Acetylsalicylic acid | 6 (14.3) |
| LVEF, mean (SD), % | 62.52 (8.3) |
AF, atrial fibrillation; BMI, body mass index; CrCL, creatinine clearance; LVEF, left ventricular ejection fraction; NOAC, new oral anticoagulants; SD, standard deviation.
Unless otherwise indicated, the data are expressed as No. (%) or median [range].
Three patients developed uncomplicated hematomas and 1 (2%), a femoral pseudoaneurysm requiring surgical treatment; 1 patient (2%) developed cardiac tamponade that required pericardiocentesis; phrenic paralysis was detected in 4 patients (9.5%) during the procedure. This complication arose during the first 18 procedures, but there were no new cases in the remainder of the interventions. This was due to the cumulative experience, specifically in the care taken to apply the energy as close as possible to the antrum, avoiding the exertion of excessive pressure by the balloon on the right veins (especially the superior vein), so that the atrial wall not be pushed closer to the phrenic nerve. In 2 patients, esophageal temperature rose (39.5°C) during the application of the laser in the left superior pulmonary vein, requiring interruption of the application. In both cases, isolation could be completed by reducing the power and modifying the ablation line.
This single-center, prospective study reports the first use of laser energy for electrical pulmonary vein isolation in Spain. The results obtained (isolation of 99% of the mapped veins, with 2 serious complications but no mortality associated with the technique) are positive and agree with those published by other authors, considering that the study period included the learning curve.6 The adaptability of the balloon catheter was excellent and, thus, ablation of most of the veins and all of the venous trunks was achieved.
The main limitations of this study are its single-center design and small sample size. Moreover, it assesses acute data on both efficacy and safety, but extended follow-up periods will be necessary to estimate the long-term efficacy of the technique.