Current European1 and American2 guidelines on the management of hyperlipidemia concur on the advisability of intensive treatment of low-density lipoprotein cholesterol (LDL-C) in patients hospitalized with acute coronary syndrome (ACS).3 However, they differ in their recommendations on post-discharge treatment. European guidelines have a therapeutic goal of LDL-C level < 70mg/dL or a reduction of LDL-C > 50%. In contrast, American guidelines, based on the efficacy shown in clinical trials,4 propose statin treatment classified according to their intensity and the theoretical percentage reduction in LDL-C they confer. As such, statins are classified into 3 categories: high-intensity (LDL-C reduction > 50%), moderate-intensity (reduction 30%-50%), and low-intensity (reduction < 30%). According to American guidelines, patients with ACS who are younger than 75 years should receive high-intensity statin therapy, while those older than 75 years should receive moderate-intensity statins. There is little focus in the guidelines on the management of atherogenic dyslipidemia (AD), which is characterized by the association of low levels of high-density lipoprotein cholesterol and high triglyceride levels, with or without increased LDL-C concentrations. Atherogenic dyslipidemia represents the main cause of residual increased cardiovascular risk once target LDL-C levels have been achieved with statins,5 but it has been little studied in patients with ACS. Our objectives were to assess the degree of compliance with current recommendations on lipid-lowering therapy on discharge in patients with a diagnosis of ACS, and to evaluate the prevalence of AD, the variables associated with this metabolic abnormality, and its influence on clinical outcomes after discharge in these patients.
We retrospectively analyzed 856 consecutive patients discharged with a diagnosis of ACS: 506 (59.1%) had ST-segment elevation and 350 (40.9%) had no ST-segment elevation but had an objective sign of myocardial ischemia (dynamic changes in the ST-segment, raised troponin, or the presence of a coronary lesion identified as the cause of symptoms). Atherogenic dyslipidemia was defined as a high-density lipoprotein cholesterol level < 40mg/dL in men and < 50mg/dL in women, with triglyceride levels ≥ 150mg/dL. We analyzed the baseline variables, the lipid profile during hospital admission and after discharge (median 3 months), and cardiovascular events–stroke or myocardial infarction–over a clinical follow-up of 12 months.
Statin therapy was prescribed in 830 patients (97%) (combined with ezetimibe in 10 patients and with fenofibrate in 18 patients). Ezetimibe alone was prescribed in 3 patients (0.4%), and fenofibrate alone in 2 (0.2%). Twenty-one patients (2.5%) received no lipid-lowering therapy. Of the 830 statin-treated patients, 570 (68.7%) received high-intensity (atorvastatin 80 mg in 77% and rotuvastatin 20 mg in 23%), 247 (29.8%) received moderate-intensity, and 13 (1.6%) received lower-intensity statins.
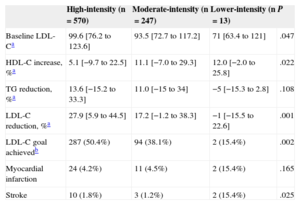
The percentage of patients treated with high-intensity statins was 65.2% among those older than 75 years and was 69% in those younger than 75 years. Use of high-intensity statins was associated with a greater reduction in LDL-C levels after discharge and a higher percentage of patients achieving therapeutic goals. The incidence of myocardial infarction or stroke during follow-up was higher in patients treated with lower-intensity statins than in those receiving moderate- or high-intensity statins (Table 1).
Baseline Patient Characteristics, Lipid Profile on Admission, and Events and Lipid Profile After Discharge, by Intensity of Statin Therapy Prescribed on Discharge
| High-intensity (n=570) | Moderate-intensity (n=247) | Lower-intensity (n=13) | P | |
|---|---|---|---|---|
| Baseline LDL-Ca | 99.6 [76.2 to 123.6] | 93.5 [72.7 to 117.2] | 71 [63.4 to 121] | .047 |
| HDL-C increase, %a | 5.1 [−9.7 to 22.5] | 11.1 [−7.0 to 29.3] | 12.0 [−2.0 to 25.8] | .022 |
| TG reduction, %a | 13.6 [−15.2 to 33.3] | 11.0 [−15 to 34] | −5 [−15.3 to 2.8] | .108 |
| LDL-C reduction, %a | 27.9 [5.9 to 44.5] | 17.2 [−1.2 to 38.3] | −1 [−15.5 to 22.6] | .001 |
| LDL-C goal achievedb | 287 (50.4%) | 94 (38.1%) | 2 (15.4%) | .002 |
| Myocardial infarction | 24 (4.2%) | 11 (4.5%) | 2 (15.4%) | .165 |
| Stroke | 10 (1.8%) | 3 (1.2%) | 2 (15.4%) | .025 |
HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; TG, triglycerides.
On multivariate analysis, the only variables independently related to the incidence of myocardial infarction or stroke were diabetes (odds ratio=2.3; P=.006) and use of lower-intensity statins compared with high-intensity statins (odds ratio=7.0; P=.002). Achieving LDL-C therapeutic goals did not affect the incidence of these events during follow-up.
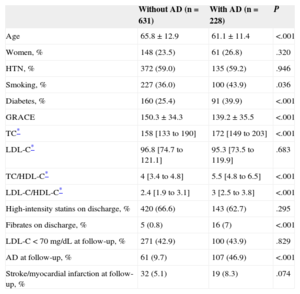
A total of 228 patients met the criteria for AD (26.5%). Compared with the non-AD group, patients with AD were younger (61.1±11.4 years vs 65.8±12.9 years; P < .001), had a higher prevalence of smoking (43.9% vs 36.0%; P=.036) and diabetes (39.9% vs 25.4%; P<.001), higher body mass index (29.5±4.3kg/m2 vs 28.4±4.6 kg/m2; P=.004), and a higher ischemic risk score according to the Global Registry of Acute Coronary Events (GRACE: 150.3±34.3 vs 139.2±35.5; P<.001) (Table 2). At follow up, a high percentage of patients in both groups achieved the therapeutic goals of LDL-C control. However, AD persisted in 46.9% of patients. Patients with AD had a higher incidence of stroke and myocardial infarction than patients without AD.
Distribution of Variables at Baseline, During Admission, and at Post-discharge Follow-up, by Presence/absence of Atherogenic Dyslipidemia
| Without AD (n=631) | With AD (n=228) | P | |
|---|---|---|---|
| Age | 65.8±12.9 | 61.1±11.4 | <.001 |
| Women, % | 148 (23.5) | 61 (26.8) | .320 |
| HTN, % | 372 (59.0) | 135 (59.2) | .946 |
| Smoking, % | 227 (36.0) | 100 (43.9) | .036 |
| Diabetes, % | 160 (25.4) | 91 (39.9) | <.001 |
| GRACE | 150.3±34.3 | 139.2±35.5 | <.001 |
| TC* | 158 [133 to 190] | 172 [149 to 203] | <.001 |
| LDL-C* | 96.8 [74.7 to 121.1] | 95.3 [73.5 to 119.9] | .683 |
| TC/HDL-C* | 4 [3.4 to 4.8] | 5.5 [4.8 to 6.5] | <.001 |
| LDL-C/HDL-C* | 2.4 [1.9 to 3.1] | 3 [2.5 to 3.8] | <.001 |
| High-intensity statins on discharge, % | 420 (66.6) | 143 (62.7) | .295 |
| Fibrates on discharge, % | 5 (0.8) | 16 (7) | <.001 |
| LDL-C < 70 mg/dL at follow-up, % | 271 (42.9) | 100 (43.9) | .829 |
| AD at follow-up, % | 61 (9.7) | 107 (46.9) | <.001 |
| Stroke/myocardial infarction at follow-up, % | 32 (5.1) | 19 (8.3) | .074 |
AD, atherogenic dyslipidemia; HDL-C, high-density lipoprotein cholesterol; HTN, hypertension; LDL-C, low-density lipoprotein cholesterol; TC, total cholesterol.
Our study highlights the lack of compliance with therapeutic goals and current recommendations on prescription of high-intensity statins in patients with ACS. The percentage reduction in LDL-C was much smaller than theoretically expected. This could have been affected by poor compliance with treatment and lifestyle modifications.
Statin therapy does not alter high-density lipoprotein cholesterol or triglyceride levels. The only drugs that have shown efficacy in increasing high-density lipoprotein cholesterol and reducing triglycerides are fibrates. However, there is little evidence on their benefits in patients with ACS and therefore recommendations on their use are not well established.
In conclusion, we found underuse of high-intensity statins in patients discharged with a diagnosis of ACS, which was not in line with current recommendations. High-intensity statins were associated with a greater LDL-C reduction and with achieving therapeutic goals, whereas lower-intensity statins were associated with a higher incidence of cardiovascular events. The prevalence of AD is high in patients admitted with a diagnosis of ACS. Treatment with moderate-intensity or lower-intensity statins is not sufficient to control the residual lipid risk in these patients. Fibrate therapy, which is underused in this population, could achieve greater control of AD and reduce the ongoing risk in these patients.