We report the uncommon case of a male patient with acute coronary syndrome (ACS) secondary to a septic embolism in the setting of infective endocarditis (IE) in a mitral valve prosthesis. To date, the literature indicates a higher frequency of this condition in aortic valve replacements. We conducted a review of the disease and of the treatment currently considered most appropriate.
The patient was a 69-year-old man whose mitral valve was replaced in 2005 with a No. 29St. Jude mechanical prosthetic mitral valve due to IE in the setting of Q fever, after he had presented to our emergency department because of an episode of syncope. On arrival, an electrocardiogram showed a complete atrioventricular block with a nodal escape rhythm at 44 bpm. The international normalized ratio (INR) was in therapeutic range. In the next few hours, while in the observation unit, the patient had typical angina, and a new electrocardiogram showed excessively discordant (2mm) ST elevation in anterior leads (V2-V4). The infarction code was activated. On arrival at the cardiac catheterization laboratory, the patient had ventricular fibrillation; he underwent immediate electrical cardioversion, which restored the previous rhythm, complete atrioventricular block, and a transitory pacemaker was implanted.
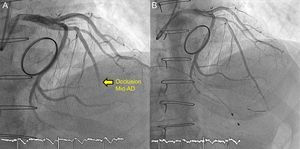
Emergency coronary angiography revealed acute occlusion of the midleft anterior descending artery, without filling of the distal vascular bed (Figure 1 and Video 1 of the supplementary material). Suspecting an embolic origin, we performed multiple thrombectomy interventions with Xport and Capturer thromboaspiration devices, with which we extracted abundant white-ish thrombotic material, with no underlying atherosclerotic plaque (Figure 1B and Video 2 of the supplementary material). Thrombolysis In Myocardial Infarction (TIMI) grade 3 flow was restored in the mid and distal anterior descending artery but with a markedly apical embolization that persisted despite percutaneous transluminal coronary angioplasty using a balloon at low atmospheres and abciximab administration at that level.
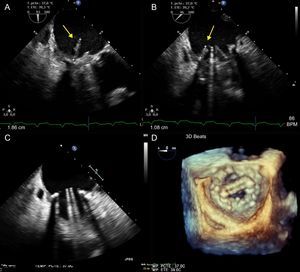
At 48hours, the patient had fever spikes and blood cultures were positive for Enterococcus faecalis. Targeted antibiotic therapy was begun with ceftriaxone and ampicillin. Transesophageal echocardiography showed a number of images compatible with vegetations in the prosthetic mitral valve, giving rise to stenotic prosthetic valve dysfunction (Figure 2A-B and Videos 3-4 of the supplementary material); the native aortic valve showed no evidence of IE. Given these findings, the patient underwent emergency surgery and a diagnosis IE with annular abscess was confirmed. A No. 27St. Jude mechanical mitral prosthetic valve was implanted. During the immediate postoperative period, the patient recovered sinus rhythm. The subsequent clinical course was favorable and he completed 6 weeks of antibiotic therapy. The results of subsequent blood cultures were negative and echocardiographic follow-up showed no images compatible with IE (Figure 2C and Figure 2D).
Acute coronary syndrome (ACS) is an early and uncommon complication of IE.1,2 Its incidence is difficult to calculate; in the series reported by Manzano et al.,1 ACS occurred as a complication of IE in 14 (2.9%) of 586 patients. Among prosthetic valves, the most frequently affected was the aortic valve.1 The syndrome is acute, developing in the first week in most patients, and is most frequently associated with aortic valve infection, severe valvular regurgitation, large periannular complications, and increased mortality.1 ACS is not related to any specific microorganism in particular but a high percentage of cases are associated with virulent pathogens such as Staphylococcus aureus.1
The injured territory is usually anterior or anterolateral,1 while presentation with ST-segment elevation is rare. The most common cause is extrinsic compression of the coronary arteries secondary to large periannular complications (pseudoaneurysms and abscesses), followed by septic coronary embolism.1,2 Other reported mechanisms are the ischemia triggered by the systemic inflammatory status, with an increase in the myocardial oxygen demand associated with febrile syndrome, anemia and/or sepsis, as well as the severe aortic regurgitation produced by myocardial ischemia due to the reduction in perfusion pressure and coronary reserve.1,2
Fibrinolytic therapy is not recommended if this complication is suspected, as it is related to a higher incidence of intracerebral hemorrhage and mortality.3,4 It is thought that this may be due to the high prevalence of silent cerebral infarctions and mycotic aneurysms due to septic embolisms, together with the bleeding risk associated with bacteremia.4 Early surgery significantly reduces embolic events.5 As a therapeutic strategy, Manzano et al.1 propose surgical referral–without previous coronary angiography–of all patients with non–ST-elevation ACS due to aortic IE and periannular complications, prior to performing transesophageal echocardiography.1 In the case of ST-elevation ACS and/or absence of periannular complication, these authors recommend the performance of coronary angiography and, if coronary occlusion is observed, they opt for balloon angioplasty and stent placement, if necessary,1 with coronary angiographic monitoring at 10 to 15 days, because of the risk of a coronary mycotic aneurysm following stent placement.1
However, other authors,4 including our group, believe that the risk involved in stent placement,1,6 in a setting of bacteremia and absence of atherosclerotic plaque, supports the benefits of thromboaspiration as the initial strategy–and if successful, the only strategy–for these patients. This approach has the added advantage of allowing the use of antiplatelet monotherapy, thus avoiding the bleeding risk associated with dual antiplatelet therapy after stenting. Finally, for patients with periannular complications and no ST segment elevation, coronary computed tomography angiography could be the alternative of choice in the study of the coronary anatomy prior to any surgical intervention.