Percutaneous coronary procedures are safe techniques that have greatly improved the prognosis of patients with ischemic heart disease. Since their introduction in cardiology, the number of percutaneous procedures has increased considerably, reaching 140 461 diagnostic procedures in 2014.1 However, despite their advantages, percutaneous procedures are not risk-free.
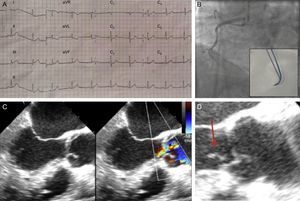
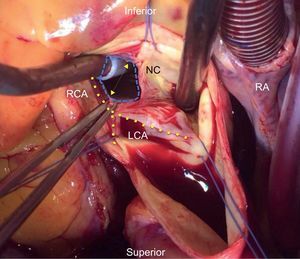
We present the case of a 63-year-old man, a former smoker with high blood pressure and dyslipidema, who was admitted to hospital with inferior ST-segment acute myocardial infarction (Figure 1A). Emergency coronary catheterization via the right radial artery revealed a lesion-free left coronary tree and a severe injury in the proximal right coronary artery (RCA), with thrombotic occlusion of the midsegment (Figure 1B). Therapeutic catheterization of the RCA proved extremely difficult due to lack of support, requiring the successive use of several catheters (JR4, AL2, and AR1) and was finally achieved with a 3D right coronary catheter (Medtronic; Minneapolis, Minnesota, United States). A hydrophilic guidewire was then inserted and the vessel was predilated with a conventional 1.5×12mm balloon at 20atm. Revascularization was achieved with 2 uncovered stents measuring 3×23mm (midsegment RCA) and 3.5×14mm (proximal RCA), yielding good angiographic and clinical results. Twenty-four hours after the procedure, the patient developed ventricular fibrillation. Sinus rhythm was restored after a 360J electric shock, advanced cardiopulmonary reanimation maneuvers, vasoactive therapy, and orotracheal intubation. Electrocardiography detected current from an inferior subepicardial injury, prompting a repeat coronary catheterization that revealed stent thrombosis. Subsequent clinical progress was slow, and the patient developed a pronounced aortic diastolic murmur that was not present on admission. Emergency transthoracic echocardiography detected an acute aortic regurgitation (AoR) with images showing nodules adhered to the ventricular surface of the aortic valve; AoR was confirmed by transesophageal echocardiography (Figure 1C–1D). Infective aortic valve endocarditis was suspected, and given the poor clinical progress, the patient was referred for surgery after 24hours. Intraoperative examination excluded endocarditis as the cause of AoR. A tear was observed at the free edge of the noncoronary aortic leaflet, associated with severe traumatic AoR and probably related to rotation of the 3D right catheter during investigation of the RCA (Figure 2). The aortic valve was beyond repair, and the patient was therefore referred for aortic valve replacement surgery, subsequently making good clinical progress.
A: Electrocardiogram showing current due to inferior subepicardial injury. B: Coronary angiogram showing thrombotic occlusion of the midsegment right coronary artery; the inset shows the 3D catheter. C: Transthoracic echocardiogram at the level of the left ventricular outflow tract at 120°, showing severe aortic regurgitation. D: Image of nodules (arrow) adhered to the ventricular plane of the aortic valve.
Intraoperative image of the aortic valve, showing perforation of the noncoronary leaflet. The 3 commissures are delimited by the sutures (discontinuous blue line). The aspirator to the left is introduced through the leaflet perforation. The aspirator to the right is placed over the ring of the injured leaflet, which is opened in the form of a V, almost obscuring the left and right coronary leaflets. The tweezers hold one edge of the perforated leaflet, which would normally join the other leaflet-half at the commissure positioned at 12 o’clock in the image. RA, right atrium; RCA, right coronary artery; LCA, left coronary artery; NC, noncoronary.
Minor complications are relatively common during percutaneous coronary procedures; however, there is a relatively low rate of potentially fatal complications such as acute arterial occlusion and cardiogenic shock. According to the 2015 Spanish Cardiac Catheterization and Coronary Intervention Registry (Registro Español de Hemodinámica y Cardiología Intervencionista), in 2014 severe complications during intervention affected 1.2% of procedures and the intervention mortality rate was just 0.4%.1
Acute traumatic AoR due to catheterization injury is an extremely rare mechanical complication. Three mechanisms have been reported for acute traumatic AoR. The most frequent is transitory regurgitation due to excessive movement of rigid catheters into the aortic arch, and the condition is relieved upon catheter withdrawal2. Irreversible acute AoR is rare and is generally related to stents implanted in the RCA ostium protruding into the aorta.3,4
Of the very few reported cases of direct catheter perforation of the coronary leaflet, most involve intervention in the RCA with Amplatz catheters.5,6 This type of complication can be prevented by careful catheter handling, especially in situations where catheterization is challenging or in patients with coronary anomalies.