Pneumococcal pneumonia (PP) and invasive pneumococcal disease (IPD) are associated with high morbidity and mortality worldwide.1 In Spain, the CORIENNE study estimated an annual incidence of pneumococcal disease of 0.28/1000 adults (age ≥ 18 years), a mortality rate of 8% among those infected, and hospitalization costs of €57 000 000.1 The incidence is even higher among adults aged 65 years or older, whose relative risk of PP or IPD is 4.8 and 4.6 times higher, respectively, than those aged 18 to 49 years,2 due to immunosenescence. Immunosuppressed patients with certain underlying diseases (Table 1) are also more susceptible to infection and their conditions are more severe with worse outcomes.1,2 The risk is cumulative and is greater in patients with multiple underlying diseases.2
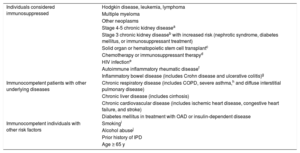
Patients Considered Immunosuppressed or Immunocompetent With Other Underlying Diseases or Risk Factors
| Individuals considered immunosuppressed | Hodgkin disease, leukemia, lymphoma |
| Multiple myeloma | |
| Other neoplasms | |
| Stage 4-5 chronic kidney diseasea | |
| Stage 3 chronic kidney diseaseb with increased risk (nephrotic syndrome, diabetes mellitus, or immunosuppressant treatment) | |
| Solid organ or hematopoietic stem cell transplantc | |
| Chemotherapy or immunosuppressant therapyd | |
| HIV infectione | |
| Autoimmune inflammatory rheumatic diseasef | |
| Inflammatory bowel disease (includes Crohn disease and ulcerative colitis)g | |
| Immunocompetent patients with other underlying diseases | Chronic respiratory disease (includes COPD, severe asthma,h and diffuse interstitial pulmonary disease) |
| Chronic liver disease (includes cirrhosis) | |
| Chronic cardiovascular disease (includes ischemic heart disease, congestive heart failure, and stroke) | |
| Diabetes mellitus in treatment with OAD or insulin-dependent disease | |
| Immunocompetent individuals with other risk factors | Smokingi |
| Alcohol abusej | |
| Prior history of IPD | |
| Age ≥ 65 y |
State in which the patient maintains eGFR < 30mL/min/1.73 m2. Estimated glomerular filtration is based on standardized measurement of serum creatinine and application of the CKD-EPI formula.
If the patient is awaiting solid organ transplant, he or she should be vaccinated 2 to 4 weeks earlier; if the patient has already undergone transplantation, the vaccination is withheld for 6 months. In patients undergoing hematopoietic stem cell transplantation, vaccination prior to transplant is not recommended, but at 3 to 6 months after the procedure.
Vaccination at least 10 to 14 days before starting treatment (preferably 4 to 6 weeks) or 3 months after completing chemotherapy or radiotherapy. Vaccination during treatment (or in the 2 weeks prior to starting) requires revaccination 3 months after treatment.
Vaccinate during the stable phase of the disease. Vaccination can take place during anti-TNF treatment but should occur before the start of treatment with methotrexate or rituximab or 1 to 3 months after finalization.
It is recommended to vaccinate on diagnosis of the disease. Vaccination is safe during treatment with immunosuppressants or biologic agents. Anti-TNF agents, immunosuppressants, or a combination of drugs reduces vaccination efficacy, and so it is preferable to vaccinate before starting these drugs.
High-risk patients with asthma (1 or more hospitalizations or visits to the emergency room; use of oral corticosteroids).
Includes active smokers with a history of smoking more than 15 pack-years without comorbidity, ex-smokers with a history of smoking for more than 20 pack-years and who have stopped smoking for more than 10 years, and any smoker, regardless of age, intensity, or exposure, with respiratory disease.
Includes problem drinkers and those with alcohol dependence syndrome. Those with consumption above the limit considered a health risk — men, more than 28 SDs/week; women, more than 17 SDs/week (SD, standard drink equivalent to 10g of pure alcohol present, for example, in a glass of wine [100mL], a glass of beer [200mL], or half a glass of whisky [25mL]). eGFR, estimated glomerular filtration rate; IPD, interstitial pneumococcal disease; OAD, oral antidiabetic agents; TNF, tumor necrosis factor.Reproduced with permission of Gonzalez-Romo et al.1
Underlying diseases with an impact on risk include cardiovascular disease (particularly congestive heart failure, ischemic heart disease, and stroke).1,2 Patients with these diseases have an incidence of PP of 2.5/1000 individuals 65 years or older, a risk of IPD 9.9 times greater than in healthy persons, and almost double the risk of hospitalization due to pneumonia. In Spain, after age and the presence of chronic obstructive pulmonary disease, cardiovascular disease is the main risk factor for respiratory deterioration in patients with PP.1 Moreover, PP notably exacerbates heart disease and its prognosis. Moreover, 32.2% of patients admitted for pneumonia have cardiovascular events in the following 30 days and, in turn, the risk of death due to these complications is 5.5 times higher, with prior heart failure being a strong independent risk factor.3
Given that vaccination is a basic strategy for the prevention of PP and IPD, it is difficult to understand why vaccination coverage is lower than desirable, even among patients at highest risk.1 Currently, 2 vaccines are available for adults: the first to become available was the pneumococcal polysaccharide vaccine (PPSV23), which was approved for patients aged 2 years or older several decades ago.1 It has not, however, been shown to be effective against PP and its effectiveness is very limited in risk groups.1 Subsequently, pneumococcal conjugate vaccines (PCV13) became available and have been used in children since 2001. Recently, its indication was extended to patients of any age. PCV13 overcomes the main drawbacks of PSV23 as it generates immune memory and a more potent and lasting immune response, avoids the phenomenon of immune tolerance, and has a stronger impact given that it acts against nasopharyngeal colonization. Limitations include the lower number of serotypes covered and the free nasopharyngeal niche resulting from vaccination.1 The CAPiTA clinical trial, with almost 85 000 participants aged 65 years or older, demonstrated the effectiveness of the PVC13 vaccine in the prevention not only of IPD (75.0%; 95.2% confidence interval [CI], 41.1%-90.9%), but also PP (45.6%; 95.2% CI, 21.8%-62.5%).4 For the primary outcome measures, efficacy was apparent soon after vaccination and the duration of the effect was maintained for at least the 4-year study duration and was greater in the 65-to 74-year-old age group.
Several recent studies in the United States, Germany, Netherlands, Italy, and Spain have found that PVC13 vaccination of adults aged 65 years or older and patients with chronic disease is cost-effective.1 A Spanish dynamic transmission model found that the use of PCV13 for 5 years in a cohort of patients aged 65 to 69 years would avoid 10 360 cases of pneumococcal disease and 699 deaths, resulting in an increase of 14 736 life-years. In terms of direct costs alone, this would correspond to a net cumulative saving of €3.8 million at fixed price (€4.9 million at current prices) and would be an efficient intervention for the Spanish National Health System.5
The Spanish Society of Cardiology, along with 17 other scientific societies, has actively participated in drafting a consensus document,1 in which any adult older than 65 years and those of any age with underlying diseases or risk factors included in Table 1, including cardiovascular disease, should receive pneumococcal vaccination, preferably, a single dose of PVC13 during their lifetime. In some cases, a dose of PPSV23 would also be indicated (Table 2), but PCV13 should always be administered first with at least 8 weeks between vaccinations. The patients who have already been vaccinated with PPSV23 could receive a dose of PVC13 after 1 year.
Recommendations for Vaccination for Adults With Underlying Disease
| Not previously vaccinated | Vaccinated previously (at least 1 year) with PPSV23 | |
|---|---|---|
| Immunosuppressedb,c (Table 1)Cerebrospinal fluid fistulasCochlear implantsAnatomical or functional aspleniaAge ≥ 65 y | PVC13 → PPSV23 (minimum interval, 8 weeks; optimum 1 y) | PVC13Revaccination with PPSV23 if more than 5 y have elapsed since first dosea |
| Immunocompetent patients < 65 y with other underlying diseases or risk factors (Table 1) | PVC13 |
Revaccination with a second dose of PVC13, allowing at least 8 weeks since the first dose if more than 5 years have elapsed since administration of the first dose of PPSV23, up to a maximum of 2 doses.
Patients who undergo hematopoietic stem cell transplant should receive 4 doses of PVC13 according to the label; a primary series of 3 doses (the first between 3 and 6 months after hematopoietic stem cell transplant and the following ones at intervals of at least 1 month) and a fourth booster dose 6 months after the third dose.
Patients in treatment with methotrexate, rituximab, abatacept, tofacitinib, or tocilizumab may require 2 doses of PVC13 vaccine and wait 1 to 3 months after finishing treatment.
Reproduced with permission of Gonzalez-Romo et al.1
Several autonomous communities fully reimburse PVC13 without cost for all adults aged 60 or 65 years and patients with some of the diseases included in the consensus document. In other autonomous communities, although there is still no public funding for all diseases of risk, patients with heart disease should be informed of the possibility of vaccination with PVC13, as indicated by the Spanish Ministry of Health, Social Services, and Equality, in the document approved by the Commission for Public Health (June 2015).6
We would like to thank the Expert Panel for drafting the consensus document on pneumococcal vaccination of adults at risk due to age and underlying disease.