Treatments to reduce low-density lipoprotein cholesterol (LDL-C) are the best tool available for secondary prevention in patients who have had an acute coronary syndrome (ACS). Consequently, guidelines recommend increasingly stringent LDL-C levels, and the previous lipid target of LDL-C < 70 has been lowered to < 55 mg/dL.1 Despite these recommendations, multicenter secondary prevention studies, such as EUROASPIRE2 and DA VINCI,3 show that these targets are reached in a low percentage of patients. Moreover, a recent study conducted in Spain reported that around 40% of postinfarction patients do not even meet the previous LDL-C target of <70 mg/dL.4 Failure to meet this goal is mainly due to underuse of the available treatments, whether the statin-ezetimibe combination or proprotein convertase subtilisin/kexin type 9 inhibitors (PCSK9i), indicated in fewer than 1% of patients.4–6
In an attempt to improve these results, a strategy was developed based on strict control and close follow-up for patients admitted to our department for ACS and designated the “post-ACS virtual lipid visit.” This study complied with the ethical principles established in the Declaration of Helsinki and was approved by the Research Ethics Committee under registration number 85.21. To summarize, the following approach was used: post-ACS patients were discharged from the hospital with high-intensity statins (unless not tolerated) and lab work was ordered for 1 month after the infarction. One month later, the patient was contacted by phone and, following a telemedicine evaluation of the test results, the lipid-lowering treatment was titrated according to the therapeutic algorithm of the consensus document from the Spanish Society of Cardiology.5 These visits were repeated each month until LDL-C was <55 mg/dL. The time to achieve the lipid target was then computed, which was the primary endpoint of this study, and the patient was released from the virtual visit schedule to continue follow-up with conventional outpatient visits. In the virtual visits, a few patients had LDL-C levels> 55 mg/dL because their health condition made it inadvisable to pursue more aggressive strategies, such as the addition of PCSK9i to their therapy.
To provide some context, this “post-ACS virtual lipid visit” approach was first implemented in 2020 at the start of the COVID-19 pandemic, which halted the normal operation of cardiac rehabilitation programs, making group activities imprudent. This “post-ACS virtual lipid visit” retained the main tasks of these programs, such as health training and cardiovascular risk factor follow-up. Moreover, by focusing on risk factors and most particularly on LDL-C, stricter control and closer follow-up of these aspects became feasible.
A total of 388 patients were consecutively admitted to our Cardiology Department for ACS in 2020. The study excluded 22 patients because they belonged to other hospital areas, 10 because they died in the first 3 months, and another 10 because they had limiting comorbidities that meant lipid control was not a priority. The other 346 patients comprised the study population. The mean age was 67.3±12.4 years, and women accounted for 31.9%. Non–ST-segment elevation ACS (59.5%) was more common than ST-segment elevation ACS (40.5%).
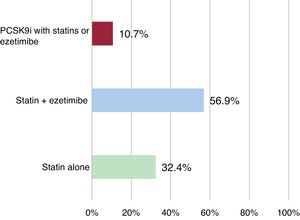
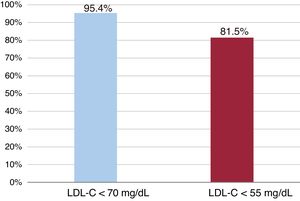
Definitive therapy for these patients consisted of high-intensity statins alone for 112 (32.4%) patients and combined therapy of statins and ezetimibe for another 197 (56.9%). The other 37 (10.7%) patients received some type of treatment that included PCSK9i along with statins or ezetimibe (figure 1). The statins most commonly prescribed were atorvastatin 80 mg and rosuvastatin 20 mg, whether alone or in combination: 295 (85.2%) of the 346 patients. With this treatment, mean LDL-C levels dropped 55.1%, from 108.4±40.6 mg/dL at ACS-related admission to 48.7±14.4 mg/dL at the completion of virtual visit follow-up. After this visit, 330 (95.4%) patients had LDL-C <70 mg/dL, and 282 (81.5%) had <55 mg/dL (figure 2). Only 16 (4.6%) patients exhibited LDL-C> 70mg, but all of them had <100 mg/dL. These results are a noticeable improvement on those recently reported in high-impact publications indicating failure to reach target lipid levels (70 mg/dL) in ≥ 40% of patients.2–4,6
The mean time required to obtain these results was only 3.2±2.1 months. Rapidly achieving the lipid target was the main purpose of this virtual visit.
The results of this study show that a more aggressive strategy in using lipid-lowering drugs (making use of combined treatment with statins-ezetimibe and PCSK9i when needed) plus closer follow-up for this specific purpose allow achievement of the guideline-recommended1 lipid target (LDL-C <55 mg/dL) in a large majority of patients (81.5%) within the first 3 months after ACS.
FUNDINGThis study was partially funded by the project (PI-0057-2017) subsidized under the Framework of the Integrated Territorial Initiative (ITI) 2014-2020 for the province of Cádiz, by the Regional Ministry of Health of the Government of Andalusia, and by the European Regional Development Fund (ERDF). Project 80% co-financed by funds from the Andalusian ERDF Operational Program 2014-2020.
AUTHORS’ CONTRIBUTIONSWe confirm that each of the authors has contributed to the study design, data collection, statistical process, and manuscript preparation.
CONFLICTS OF INTERESTNone.