Telemedicine has been shown to improve access to health care by overcoming geographical inequities and adapting to situations such as the current coronavirus disease 2019 (COVID-19).1 Although the available evidence is scarce, we believe that telemedicine, in addition to improving the efficiency of health care systems, could be associated with better health outcomes.
Multidisciplinary programs that integrate different levels of care represent the best model for the management of patients with heart failure (HF).2 Telemedicine has been shown to be effective in the clinical follow-up of these patients and contributes to their clinical stability by the optimization of treatment and the early identification of decompensation, thereby reducing hospitalizations and mortality.3 The integration of electronic medical records across all health care levels allows clinical information to be shared, thus improving the organization of demand for care.4 This aspect is particularly relevant in relation to chronic diseases characterized by frequent decompensations, such as HF.
A recent publication described the impact of incorporating a universal electronic consultation program (started in 2013) on waiting times in care and health outcomes (e-consultation).5 This initiative was the first step in the outpatient care process for patients referred to a cardiology service by primary care (PC) physicians using an integrated electronic medical record. The results of e-consultation were compared with those of the previous period of exclusive face-to-face consultation (from 2008 to 2012). There was a significant reduction in waiting times, with a lower rate of hospital admissions, emergency department visits, and mortality in the year following the consultation.5 We proposed that e-consultation could lead to better and faster risk stratification, which could in turn allow treatment optimization. This proposal was partly confirmed by our findings.
We conducted an observational retrospective quality-of-care study that analyzed the information recorded in the management accounting unit of our health area. The information obtained was anonymized and did not involve any risk to patients. Informed consent was waived due to the large number of patients and the length of time involved.
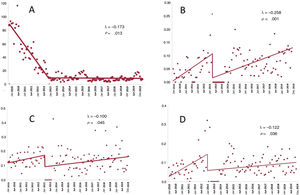
The aim of this letter was to describe the clinical characteristics of HF patients referred for consultation by PC physicians, as well as the impact of implementing e-consultations on waiting times and health outcomes in patients with a history of HF. We used interrupted time series analysis to investigate the impact of e-consultation on consultation waiting times, emergency room visits, hospital admission, and mortality 1 year after consultation.6
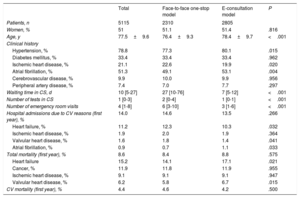
A total of 10.8% of patients referred for consultation had a previous diagnosis of HF, with a decreasing trend between 2010 (11.2%) and 2019 (8.6%). The characteristics of patients with HF referred for consultation by PC physicians are shown in table 1. In general, patients were elderly, had a high prevalence of comorbidities (more than 50% had atrial fibrillation), had a low likelihood of their demand for care being resolved via e-consultation (9.2%), and had a high need for successive consultations during the initial face-to-face consultation period (60.3%) and after the implementation of the e-consultation program (72.7%). The table also shows the progress of the patients with a previous diagnosis of HF (need for emergency room visits, hospital admission, and mortality 1 year after consultation). The interrupted time series analysis showed a sharp reduction in waiting times at the start of the e-consultation program. Waiting times had already been decreasing in previous years under the 1-stop approach to consultations. There was also a significant reduction in emergency room visits, hospital admissions, and mortality (figure 1). The increased rate of emergency room visits by patients with HF observed during the in-person period of 1-stop consultations underwent a sharp fall (9.9%; 95% confidence interval [95%CI], 5.9%-13.9%) after the implementation of e-consultation, even though the previous annual growth rate remained unchanged. There was also a significant reduction in the hospital admission rate (10.0%; 95%CI, 5.1%-14.9%) and mortality (12.2%; 95%CI, 6.4%-18.0%) after the implementation of e-consultation. This rate remained relatively stable after its implementation.
Characteristics of patients with heart failure under each consultation model
| Total | Face-to-face one-stop model | E-consultation model | P | |
|---|---|---|---|---|
| Patients, n | 5115 | 2310 | 2805 | |
| Women, % | 51 | 51.1 | 51.4 | .816 |
| Age, y | 77.5±9.6 | 76.4±9.3 | 78.4±9.7 | <.001 |
| Clinical history | ||||
| Hypertension, % | 78.8 | 77.3 | 80.1 | .015 |
| Diabetes mellitus, % | 33.4 | 33.4 | 33.4 | .962 |
| Ischemic heart disease, % | 21.1 | 22.6 | 19.9 | .020 |
| Atrial fibrillation, % | 51.3 | 49.1 | 53.1 | .004 |
| Cerebrovascular disease, % | 9.9 | 10.0 | 9.9 | .956 |
| Peripheral artery disease, % | 7.4 | 7.0 | 7.7 | .297 |
| Waiting time in CS, d | 10 [5-27] | 27 [10-76] | 7 [5-12] | <.001 |
| Number of tests in CS | 1 [0-3] | 2 [0-4] | 1 [0-1] | <.001 |
| Number of emergency room visits | 4 [1-8] | 6 [3-10] | 3 [1-6] | <.001 |
| Hospital admissions due to CV reasons (first year), % | 14.0 | 14.6 | 13.5 | .266 |
| Heart failure, % | 11.2 | 12.3 | 10.3 | .032 |
| Ischemic heart disease, % | 1.9 | 2.0 | 1.9 | .364 |
| Valvular heart disease, % | 1.6 | 1.8 | 1.4 | .041 |
| Atrial fibrillation, % | 0.9 | 0.7 | 1.1 | .033 |
| Total mortality (first year), % | 8.6 | 8.4 | 8.8 | .575 |
| Heart failure | 15.2 | 14.1 | 17.1 | .021 |
| Cancer, % | 11.9 | 11.8 | 11.9 | .955 |
| Ischemic heart disease, % | 9.1 | 9.1 | 9.1 | .947 |
| Valvular heart disease, % | 6.2 | 5.8 | 6.7 | .015 |
| CV mortality (first year), % | 4.4 | 4.6 | 4.2 | .500 |
CV: cardiovascular; CS: cardiology service.
Unless otherwise indicated, values are expressed as mean ± standard deviation or median [interquartile range].
These results were obtained in a large series of patients with a diagnosis of HF. They show that introducing an e-consultation program to manage consultations requested by PC physicians is safe and leads to reduced waiting times because of the significant reduction in the need for urgent care, hospital admissions, and mortality in a group of patients at high risk of clinical instability. The effect of the implementation of this e-consultation program did not prevent a subsequent increase in the annual rate of urgent consultations, hospital admissions, and mortality. Nevertheless, the increase was smaller than that observed during the face-to-face consultation period, especially regarding the risk of hospital admission and mortality. Our results shows that the implementation of e-consultation to manage the demand for care in HF patients improves risk stratification and leads to faster patient treatment by reducing waiting times.
FUNDINGNone declared.
AUTHORS’ CONTRIBUTIONSAll authors participated in data collection, data analysis, reviewing the results, and drafting, revising, and giving final approval to the manuscript.
CONFLICTS OF INTERESTNone declared.