Minimal ST-elevation often leads to inappropriate diagnoses and delayed interventions. Recent studies have shown that between 11% and 23% of infarctions do not reach the cutoff for accepted electrocardiographic criteria for infarction, and the absence of such criteria is not associated with a more favorable prognosis.1,2 The main objective of this study was to analyze the prevalence of reciprocal changes (RC) as a diagnostic tool in myocardial infarction with minimal ST-elevation.
The study was based on a prospective registry of 480 consecutive patients with a definitive diagnosis of infarction who underwent emergency coronary angiography as part of a systematic primary angioplasty program between 2009 and 2011. The present study comprised 75 patients with a maximum ST-elevation of 0.01 to 0.1mV and who could be assessed for RC. The indication for catheterization was based on persistent symptoms of ischemia. No patient received thrombolysis during the study period.
Reciprocal changes were defined as J point depression ≥ 0.05mV in the TP segment, in at least 1 lead other than the aVR lead. All patients provided informed consent prior to participation.
Variables were compared using the chi-square test, the Fisher exact test, and the Mann-Whitney U test. The variables associated with RC with P < .1 (age, site, multivessel disease) were included in the multivariate logistic regression model to assess whether they were independently associated.
In total, 51 patients had RC (prevalence 68%, 95% confidence interval [95%CI], 57%-79%), which was attributed to an ischemic cause in all of them. In 27 patients, a depression ≥ 0.1 mV was observed and, in all patients except 1, the slope was horizontal or decreasing.
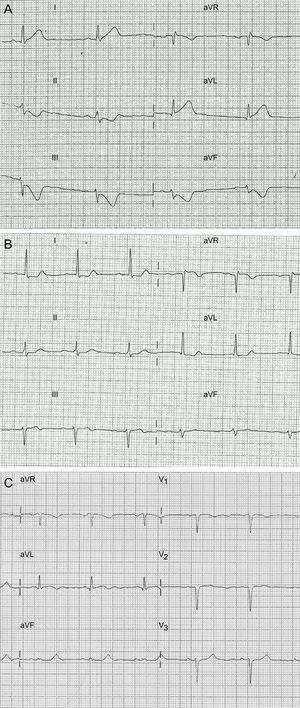
Among the 24 remaining patients, 17 showed an ST-depression of 0.01-0.04mV (n = 15) or negative or symmetric T waves (n = 10). Overall, 68 patients had some sort of RC that supported diagnosis (91%; 95%CI, 84%-97%) (Figure).
The Table shows the characteristics of the groups according to the presence of RC. In all patients, initial thrombolysis in myocardial infarction (TIMI) flow was 0/1 or creatinine kinase was elevated to more than 3 times the upper limit of normal. Although the enzyme concentrations were similar, patients with RC showed a tendency toward a higher incidence of heart failure during hospitalization (31% vs 12%; P = .080).
Clinical and Angiographic Findings in Patients in the Study According to the Presence of Reciprocal Changes
| No RC (n = 24) | RC (n = 51) | P | |
|---|---|---|---|
| Baseline characteristics | |||
| Age, y | 58 [48-69] | 66 [55-75] | .055 |
| Male sex | 17 (71) | 40 (78) | .472 |
| Hypertension | 14 (58) | 29 (57) | .904 |
| Diabetes mellitus | 5 (21) | 13 (25) | .660 |
| Dyslipidemia | 10 (42) | 27 (53) | .362 |
| Current smoker | 16 (67) | 28 (55) | .334 |
| Chronic kidney disease | 2 (9) | 8 (16) | .485 |
| Prior myocardial infarction | 4 (17) | 7 (14) | .740 |
| Clinical presentation | |||
| Anterior site | 8 (33) | 5 (10) | .02 |
| Symptoms-to-door time, min | 151 [60-582] | 170 [85-227] | .931 |
| Door-to-balloon time, min | 111 [58-187] | 85 [66-132] | .378 |
| Q wave | 9 (37) | 18 (35) | 1.0 |
| Corrected QT > 450 ms | 7 (29) | 15 (30) | 1.0 |
| LVEF, % | 62 [47-72] | 59 [50-67] | .327 |
| Maximum troponin I, ng/mL | 18 [12-69] | 26 [12-49] | .782 |
| Maximum CK, U/L | 930 [524-2140] | 972 [526-1573] | .857 |
| Angiography findings | |||
| Culprit artery | .448 | ||
| Anterior descending | 8 (33) | 9 (18) | |
| Circumflex | 6 (25) | 16 (31) | |
| Right coronary | 10 (42) | 25 (49) | |
| Venous graft | 0 (0) | 1 (2) | |
| Basal TIMI flow 0/1 | 18 (82) | 41 (85) | .731 |
| Multivessel disease | 10 (42) | 32 (63) | .086 |
CK, creatinine kinase; LVEF, left ventricular ejection fraction; RC, reciprocal change; TIMI, thrombolysis in myocardial infarction.
Data expressed as no. (%) or median [interquartile range].
In the analysis by infarction site, the prevalence of RC was 38% (95%CI, 8%-69%) in anterior acute myocardial infarction, 70% (95%CI 35%-100%) in lateral or inferobasal infarction, and 75% (95%CI, 63%-87%) in inferior infarction (P = .041). In the multivariate analysis, nonanterior site was independently associated with the presence of RC (odds ratio = 4.6; 95%CI, 1.3-16.1; P = .017).
An important finding in this study of patients with minimal ST-elevation treated with systematic primary angioplasty is that two-thirds of the patients with borderline electrocardiogram and no diagnosis of myocardial infarction showed reciprocal depression ≥ 0.05 mV and 91% had some type of RC that was useful for early diagnosis of infarction.
One aspect worthy of discussion is whether to adjust the cutoff for defining RC in patients with borderline electrocardiogram. The ST segment should, in normal conditions, be isoelectric or show a depression < 0.05mV. Classical studies of ST-elevation myocardial infarction show reciprocal depression ≥ 0.1 mV in approximately 60% of inferior infarctions and 30% of anterior infarctions.3,4 In a study of 126 infarctions with minimal ST elevation, Jang et al1 reported RC in 58%. In our study, lowering the cutoff to 0.05mV enabled detection of RC in 68% of patients compared with 36% when a cutoff of 0.1mV was used. Along these lines, it has been observed that a certain degree of ST depression is an almost universal finding in inferior infarction and is very uncommon in pericarditits.5,6 These arguments would therefore support the use of a more lax criterion (≥ 0.05 mV) for a condition in which diagnostic sensitivity is of the utmost importance.
Moreover, the presence of RC may have prognostic implications. Some studies have associated RC with the extent of myocardium at risk and with multivessel disease.3 In our series, the patients with RC showed a tendency toward more multivessel disease and a greater incidence of heart failure during hospitalization.
Among the limitations of the study, of note is the absence of a control group, although the aforementioned studies have shown that RC are uncommon in other entities and their presence would be more specific for infarction. We did not include patients not undergoing coronary angiography. Nevertheless, the high proportion of patients with minimal ST-elevation suggests that the sample is representative of the study population.
In conclusion, RC is extremely useful for identifying and enabling early treatment of patients with chest pain and minimal ST-elevation in inferior and lateral leads. In anterior infarction, the absence of RC is common, and therefore diagnosis should consider other clinical, electrocardiographic, and imaging criteria.