To the Editor,
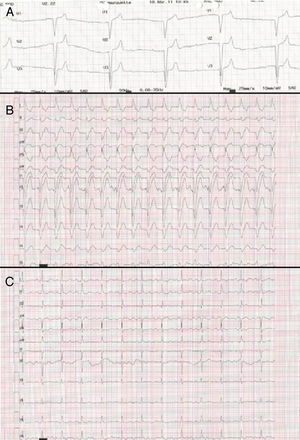
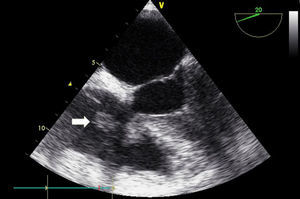
A 76-year-old woman presented with fever that began 2 days previously, along with general malaise and dyspnea. She had a history of hypertension and dyslipidemia, and was undergoing dialysis for chronic end-stage renal failure via a permanent internal jugular vein catheter. Laboratory studies revealed leukocytosis with left shift, along with white blood cells and bacteria in urinary sediment. She was admitted to hospital with a diagnosis of febrile syndrome probably due to a urinary tract infection, and antibiotic treatment was initiated with levofloxacin. Four days after admission, she had a long episode of nausea and sweating. Her blood pressure was raised and physical examination revealed bradycardia with a left parasternal systolic murmur. An electocardiogram (Figure 1A) revealed a widened QRS interval with an escape rhythm of 30 bpm due to third-degree atrioventricular block (AVB). A decision was therefore taken to immediately implant a temporary pacemaker via the jugular vein. A few hours later the patient recovered her normal rhythm but with first-degree AVB and complete left bundle-branch block (Figure 1B). Due to the febrile syndrome and a continued murmur, a transthoracic echocardiogram was carried out. Two large vegetations were observed on the tricuspid valve; the most mobile measured 10×16mm and was anchored to the free edge of the valve (Figure 2), while a second, smaller growth was observed at the insertion of the septal leaflet. A transesophageal echocardiogram undertaken to complete the study confirmed the earlier findings and ruled out involvement of the left valves or other complications. Three separate blood cultures revealed growth of methicillin-sensitive Staphylococcus epidermidis and a urine culture was negative. Infectious endocarditis due to S epidermidis was diagnosed, probably secondary to catheter infection. On this basis, treatment was initiated with gentamicin and cloxacillin, and the dialysis catheter was surgically removed. Electrocardiographic monitoring over the next 72h revealed progressive narrowing of the QRS interval until it reached 86ms, with persistence of first-degree AVB (Figure 1C). After a week of treatment with antibiotics, blood cultures were negative and no new conduction abnormalities were observed in the electrocardiogram. Therefore, the temporary pacemaker was removed. The catheter tip culture was positive for S epidermidis. After 5 days of combined antibiotic therapy, gentamicin was suspended and treatment continued with cloxacillin alone. The patient's condition followed an unfavorable course with worsening renal failure and development of systemic congestion, resulting in death 23 days later.
Figure 1. A, Third-degree atrioventricular block with widened QRS intervals and escape rhythm. B, A few hours after implantation of a temporary pacemaker, first-degree atrioventricular block is visible alongside complete left bundle-branch block. C, Three days later, the electrocardiogram reveals first-degree atrioventricular block with narrowed QRS intervals.
Figure 2. Transesophageal echocardiogram revealing a large vegetation on the free edge of the tricuspid valve (white arrow) and a smaller vegetation on the septal leaflet.
Severe conduction disorders are a rare manifestation of infectious endocarditis. According to data from patient registries, their occurrence is between 1% and 15% of cases. They are associated with worse prognosis due to an increased risk of embolus and with higher mortality. Conduction abnormalities are caused by spread of the infection from the valves to the conduction pathways and are generally associated with perivalvular complications. Third-degree AVB is most often associated with disease affecting the left valves (aortic, 36%; mitral, 33%) and cases of tricuspid endocarditis are rare (2%).1 This is because of the anatomical relationship with the atrioventricular node, which is situated at the centre of Koch's triangle, close to the noncoronary aortic leaflet and the anterior mitral leaflet; the tricuspid septal leaflet, on the other hand, is located at the base of Koch's triangle. In a study of patients with endocarditis and complete AVB, pathology workup revealed the presence of an infection, usually accompanied by abscesses and fistulas, that affected the conduction pathways; in cases involving paroxysmal AVB, inflammation was observed at this level, which would explain the reversibility of the event.2 Electrocardiographic monitoring is important in patients with endocarditis, as the appearance of conduction abnormalities can alert us to the appearance of perivalvular complications; similarly, once a conduction block has been detected, its disappearance in less than a week indicates a good response to antibiotic treatment.3
Right-sided endocarditis is an underdiagnosed condition, probably due to its atypical clinical presentation,4 although vegetations can be readily observed even by transthoracic echocardiography.5 The case described here is exceptional in that it involved isolated tricuspid endocarditis appearing with complete AVB and left bundle-branch block that was reversed upon treatment with antibiotics. Cases of conduction abnormalities in association with tricuspid valve endocarditis have rarely been described in the literature, although there appears to be a tendency for the block to be reversed with medical treatment, without the need to implant a permanent pacemaker or resort to surgery.6
.
Corresponding author: noemu83@hotmail.com