Unroofed coronary sinus is a rare form of atrial septal defect (ASD) in which the left atrium, coronary sinus, and right atrium are connected due to a defect in the roof of the coronary sinus.1–4 The condition can remain undiagnosed because the clinical manifestations are nonspecific and the anatomy is hard to identify by transthoracic echocardiography.2,3,5 The standard treatment is surgical closure.3,4
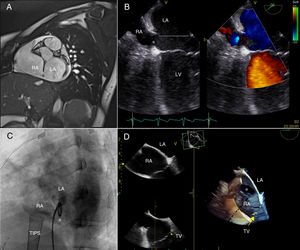
A 17-year-old woman with liver failure secondary to cavernous transformation of the portal vein was referred for cardiological assessment before liver transplant. The patient had been fitted with an intrahepatic transjugular portosystemic shunt to control portal hypertension. Transthoracic echocardiography revealed dilatation of the right ventricle, raising suspicion of ASD associated with unroofed coronary sinus. Magnetic resonance imaging confirmed the complete absence of the coronary sinus roof, accompanied by dilatation of the coronary sinus ostium and a Qp:Qs ratio = 1.9 (Figure 1A).
A. Magnetic resonance image, sagittal view. B, Transesophageal echocardiography 4-chamber view, showing the coronary sinus ostium and the completely unroofed coronary sinus (dotted line in the left atrium). C, Angiography in the left anterior oblique view, showing the pigtail catheter in the left atrium through the coronary sinus ostium (asterisk). D, 3D transesophageal echocardiography, left atrial view. *, coronary sinus ostium; LA, left atrium; LV, left ventricle; RA, right atrium; TIPS, transjugular portosystemic shunt; TV, tricuspid valve.
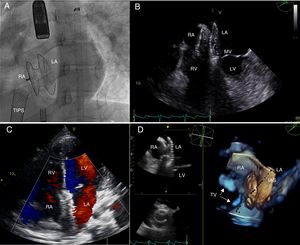
After a multidisciplinary assessment, the decision was taken to close the defect percutaneously, due to the liver failure and the patient's poor clinical status. Defect anatomy was defined by transesophageal echocardiography (TEE) and left-atrium angiography (Figure 1B and C and videos 1 and 2 of the supplementary data). The size of the coronary sinus ostium defect (in the inferoposterior region of the interatrial septum) was measured by angiography and 3D TEE (Figure 1D and video 3 of the supplementary data). The maximum initial diameter was 17-18mm, and the stop-flow diameter determined by fluoroscopy and TEE was 20-21mm. The device selected for the procedure was a 21mm Figulla-Flex II ASD occluder (FFO, Occlutech GmbH; Jena, Germany), which was advanced through a long sheath to the left atrium. The left disc was opened in the left atrium, the device waist was positioned in the coronary sinus ostium, the right disc was opened in the right atrium, and the device was released without incident. Nevertheless, some minutes later, the device migrated to the left ventricle and was retrieved by retrograde capture from the femoral artery. The atrial defect subsequently measured 23-24mm on TEE, with the increase possibly due to the passage of the device through the defect and the rigid guidewire used for the second implant. For the second attempt, a 27mm Figulla-Flex II device was selected and was released without subsequent events (Figure 2A-D and videos 4-6 of the supplementary data).
A, Fluoroscopy in the left anterior oblique view. B, 2D transesophageal echocardiography, 4-chamber view; the device can be seen occluding the coronary sinus ostium. C, color Doppler transthoracic echocardiography in 4-chamber view, showing the absence of transatrial shunting. D, 3D transesophageal echocardiography in the superoanterior view. IAS, interatrial septum; LA, left atrium; LV, left ventricle; MV, mitral valve; RA, right atrium; RV, right ventricle; TIPS, transjugular portosystemic shunt; TV, tricuspid valve.
We detected no interference with the atrioventricular valves, and the patient maintained sinus rhythm. The device eliminated the left-to-right transatrial shunt, and the coronary veins continued to drain into the left atrium (the coronary sinus remained unroofed). The right ventricular enlargement gradually regressed during follow-up, and the device remained in the correct position after 6 months.
Unroofed coronary sinus accounts for less than 1% of ASDs.1 The condition can occur alone or together with other cardiac defects such as persistent left superior vena cava (LSVC), tricuspid atresia, and some forms of heterotaxy.1–5
Kirklin and Barratt-Boyes proposed an anatomical classification of unroofed coronary sinus, which is still in use. Types I and II denote complete unroofed coronary sinus, either with (type I) or without (type II) persistent LSVC; types III and IV are partial forms in which the coronary sinus is unroofed in the midportion or terminal portion, respectively.2 The case described here is an example of type II unroofed coronary sinus, occurring with dilatation of the coronary sinus ostium.
Although most children with unroofed coronary sinus are asymptomatic, it is important to diagnose this ASD because of its possible long-term complications. These complications include cyanosis due to right-to-left shunting, pulmonary hypertension, brain abscess, and paradoxical embolism.1–5
Percutaneous closure of unroofed coronary sinus is a valid alternative to surgery, first described in 2003.4,6 Since then, a handful of articles have reported percutaneous closure of unroofed coronary sinus with a covered stent or the Amplatzer septal occluder.5,6 Closure with a stent carries a risk of obstructing coronary venous drainage.6 Moreover, since the patient described here had a completely unroofed coronary sinus without LSVC, stent closure was not an option due to the lack of anchorage sites. We therefore opted for closure of the coronary sinus ostium with a percutaneously placed device, despite the small left-to-right short circuit inherent to this procedure due to the direct drainage of the coronary veins into the left atrium, which causes a slight desaturation.
Although surgery continues to be the treatment of choice for the closure of coronary sinus ASDs, the percutaneous approach is developing rapidly. In specific cases, this approach provides a valid, safe, and less invasive alternative.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2019.03.014.