Stress echocardiography is used for the diagnosis and prognostic assessment of patients with known or suspected coronary artery disease. In Spain, stress echocardiography is generally carried out in the hospital setting. The latest European Society of Cardiology (ESC) guidelines on chronic coronary syndromes recommend that patients with a pretest probability> 15% should initially be tested by noninvasive functional imaging for myocardial ischemia or coronary computed tomography angiography.1 The ESC guidelines indicate that the choice of the initial noninvasive test used for diagnosis and to establish prognosis should be based on availability and local expertise. The new recommendation is principally spurred by the low positive and negative predictive value of conventional exercise electrocardiography compared with imaging techniques.2
At our center, with a catchment population of 530 000 people, implementation of the new recommendation has led to an increase in the number of stress echocardiograms and a correspondingly sharp reduction in the number of conventional exercise electrocardiography tests. This change has required an operational reorganization of the cardiac imaging unit.
In response to the growing demand for stress echocardiography, a dedicated program has been established at a specialized nonhospital health center that previously carried out conventional treadmill exercise electrocardiography tests. The nonhospital center is located 5km from the referral hospital, and the estimated ambulance transfer time is normally 10 to 15minutes.
Here, we report the analysis of the first 200 patients referred to the nonhospital center for stress echocardiography to diagnose coronary artery disease or assess its prognosis.
Studies were performed by a nurse and a cardiologist with expertise in cardiac imaging, and practitioners were trained in stress echocardiography and advanced life support. The stress echocardiography service is equipped with a defibrillator, oxygen equipment, an aspirator, and drugs and instruments required for advanced life support, including all material needed for orotracheal intubation.
All tests were performed on a treadmill using the Bruce method or the modified Bruce method. To increase diagnostic efficiency, a 1mg intravenous dose of atropine was given to patients with no contraindications and with a very low estimated probability of achieving submaximal heart rate due to low functional capacity or nonwithdrawal of rate-reducing medication.3 Contrast echocardiography was used in all patients with a suboptimal acoustic window.
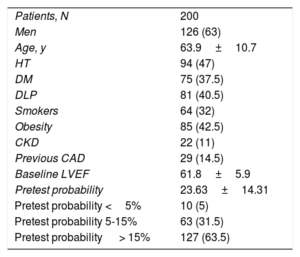
Baseline patient characteristics are summarized in table 1. Mean pretest probability according to the 2019 ESC guidelines1 was 23.63%±14.31%. Of the patients studied, 127 (63.5%) had a pretest probability> 15%. No adverse events were recorded during the tests.
Baseline characteristics
| Patients, N | 200 |
| Men | 126 (63) |
| Age, y | 63.9±10.7 |
| HT | 94 (47) |
| DM | 75 (37.5) |
| DLP | 81 (40.5) |
| Smokers | 64 (32) |
| Obesity | 85 (42.5) |
| CKD | 22 (11) |
| Previous CAD | 29 (14.5) |
| Baseline LVEF | 61.8±5.9 |
| Pretest probability | 23.63±14.31 |
| Pretest probability <5% | 10 (5) |
| Pretest probability 5-15% | 63 (31.5) |
| Pretest probability > 15% | 127 (63.5) |
CAD, coronary artery disease; CKD, chronic kidney disease; DLP, dyslipidemia; DM, diabetes mellitus; HT, hypertension; LVEF, left ventricular ejection fraction.
Unless indicated otherwise, data are expressed as no. (%) or mean±standard deviation.
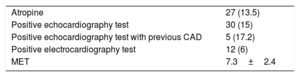
The stress echocardiography results are summarized in table 2. Test results were positive in 15% of patients (n=30). Of these patients, only 40% (n=12) had positive results in the exercise electrocardiography test. Of the positive echocardiography tests, 4 could not be evaluated electrocardiographically due to the presence of underlying conduction disorders.
Exercise test variables
| Atropine | 27 (13.5) |
| Positive echocardiography test | 30 (15) |
| Positive echocardiography test with previous CAD | 5 (17.2) |
| Positive electrocardiography test | 12 (6) |
| MET | 7.3±2.4 |
CAD, coronary artery disease; MET, metabolic equivalents.
Data are expressed as no. (%) or mean±standard deviation.
Atropine was given to 27 patients (13.5%) in accordance with the safety warnings for this drug. The indications for atropine were as follows: 22 patients took beta-blockers on the day of the test or the day before, 1 was under treatment with more than 1 rate-reducing drug, and 4 were not taking rate-reducing medication but had low functional capacity. No adverse effects were observed.
In Spain, stress echocardiography is the most widely available imaging test for the detection of ischemia. Restricting this test to the hospital setting limits the capacity of health services to respond to the growing demand for this procedure.
In our experience, the use of stress echocardiography in a specialized nonhospital center staffed with trained personnel is safe, allows health services to respond to the growing demand for this test, and increases diagnostic efficiency.