Cardiac involvement is not uncommon in systemic inflammatory diseases. When such diseases present with a cardiac manifestation, it is generally in the form of pericarditis, which is usually acute and recurrent.1 We report a case of adult Still's disease presenting clinically as severe acute pericarditis.
A 33-year-old man presented to our hospital in April 2008 with chest pain suggestive of pericarditis and a temperature of 38°C. Relevant medical history included smoking. Since 1999, he had been diagnosed on multiple occasions with acute idiopathic pericarditis requiring multiple hospital admissions, which was treated mostly with high dose nonsteroidal anti-inflammatory drugs, and occasionally with colchicine. These episodes generally occurred with no pericardial effusion or a mild effusion at most. There was usually an associated increase in acute phase reactants and typical electrocardiographic changes during the acute episode.
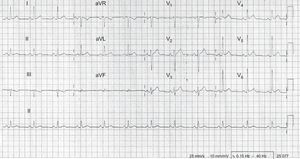
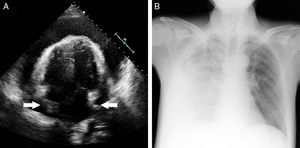
He reported chronic fatigue but no osteoarticular symptoms. Heart sounds were regular, and there was no audible pericardial rub. Pulsus paradoxus was not detected, and there were no signs of congestion or hemodynamic compromise. Electrocardiography showed a sinus rhythm of 65 bpm, with changes typical of pericarditis (Figure 1). On chest radiograph, there were no pulmonary infiltrates and the cardiac shadow was of normal size and shape. Blood tests on admission showed normal cardiac enzymes and brain natriuretic peptide; there was leukocytosis and a significant increase in C-reactive protein, erythrocyte sedimentation rate, ferritin, and liver transaminases. Serology was performed for hepatotropic viruses and HIV, among others, as well as for atypical bacteria, with negative results. Autoimmune study, tumor markers, and Mantoux test were negative. Serial peripheral blood cultures were persistently negative. Initial echocardiography revealed a mild pericardial effusion. On the fourth day of admission, with worsening symptoms, repeat echocardiography was performed, which showed severe pericardial effusion with signs of hemodynamic compromise (Figure 2A). Emergency pericardiocentesis was performed, which drained 500mL of serosanguinous fluid compatible with an exudate (leucocytes, 15 000/¿L, 75% polymorphonuclear neutrophils; protein, 58g/L; lactate dehydrogenase, 2286 IU/L; pH 7.41; glucose and adenosine deaminase, normal; and bacterial culture and Ziehl stain, negative, with no other findings of note on cytological and biochemical testing).
Subsequently, the patient had spiking fevers, one of which was associated with tachypnea, severe dyspnea, and arterial desaturation. Urgent echocardiography ruled out recurrence of the pericardial effusion, but led to the diagnosis of a massive right pleural effusion (Figure 2B) requiring urgent thoracocentesis. This drained 2000mL of serosanguinous fluid, which was also exudative. Computed tomography of the chest, abdomen, and pelvis was performed to rule out an underlying neoplastic or hematological disease, and no significant abnormalities were found.
Over the following days, the patient improved and was discharged from hospital on colchicine, ibuprofen, and aspirin, at high doses. Two weeks later, he was readmitted with signs of pericarditis, a temperature of 38°C, fatigue, cough, and odynophagia. On echocardiography, no significant pericardial effusion was seen. His chest pain improved, but he began to complain of discomfort in the hips and left elbow. During this hospital stay, a nonpruritic salmon-colored macular rash was noted.
In light of the overall clinical picture, there was a high suspicion of a systemic inflammatory disease and, after a review of the available literature, a diagnosis was made of adult Still's disease with an indolent, atypical presentation and clinical course. Therefore, we decided to start methotrexate therapy.
Following that episode, the patient had mild recurrences of pericarditis, usually in the context of having stopped treatment for no particular reason. Therefore, we decided to give intramuscular methotrexate. Since then, with treatment adherence ensured, he has required no further hospital admissions. At nearly 8 years since diagnosis, there have been no signs of pericardial constriction or other cardiovascular complications on clinical review or on echocardiography at follow-up.
Adult Still's disease is a rare inflammatory disease of unknown etiology, which mainly affects young adults. It is characterized by high fever, evanescent salmon-colored maculopapular rash, and arthritis, often with associated odynophagia, lymphadenopathy, hepatosplenomegaly, and pleuropericarditis. The diagnosis is made by exclusion of other causes.2 Pericarditis is the most common cardiac manifestation and is subclinical in up to 50% of patients. Cardiac tamponade, constrictive pericarditis, and endocarditis are extremely rare. Treatment of this disease is not well established. Between 20% and 25% of patients respond to treatment with high dose salicylates, which should therefore be the first-line treatment. In severe cases, glucocorticoids are used (50% to 70% of cases). However, in the context of pericarditis, their use has been independently associated with risk of recurrence.3,4 In approximately one third of cases, the addition of methotrexate or other disease-modifying drugs is required.
Prognosis depends on an early diagnosis and starting the appropriate treatment.
In the case reported here, the patient had recurrent pericarditis with an unusual and complicated course, which contributed to a late but accurate diagnosis, according to current criteria,2 of adult Still's disease.