Hypersensitivity or intolerance to aspirin occurs in 1.5% of patients with coronary artery disease.1 Despite the availability of desensitization protocols, such procedures are rarely undertaken. Desensitization is therapeutically challenging in patients with acute coronary syndrome who require dual antiplatelet therapy to reduce adverse cardiovascular effects2 and in those patients requiring stent implantation.
Aspirin hypersensitivity arises because the inhibition of the enzyme cyclooxygenase (COX) shifts arachidonic acid metabolism toward hyperproduction of cysteinyl leukotrienes, which are the compounds that cause the observed symptoms. Aspirin hypersensitivity can manifest as exacerbated respiratory disease and urticaria or angioedema, but there has been no convincing report of immunoglobulin E-mediated anaphylaxis.3
Protocols for aspirin desensitization were developed in the 1980s and protocols for patients with coronary artery disease were introduced in 2000. The early protocols were carried out in stable patients under treatment with antihistamines and lasted several days. Current protocols take 2-5hours and can be used with patients with unstable disease. A recent meta-analysis summarized the features of current protocols and included the results of an international survey of cardiologists; in the survey, 42% of respondents reported that they carried out ASA desensitization protocols, a figure higher than that for Spain.4
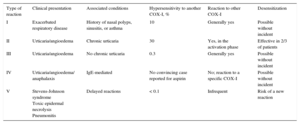
We have evaluated the short- and long-term efficacy and safety of the aspirin desensitization protocol used at our center. The first step is to identify the type of reaction the patient has experienced (Table 1).5 Our desensitization protocol is carried out with the help of the Allergy Service and is adapted from Dalmau et al.6 Patients are given oral aspirin every 15 to 20minutes in progressively increasing doses, beginning at 0.1mg and with a final dose of 100mg. The doses (0.1, 0.3, 1, 10, 25, 50, 100mg) are obtained by dilution from a 900mg stock of lysine acetylsalicylate (doses and equivalence to aspirin tablets agreed with the Pharmacy Service). The lysine acetylsalicylate is administered without antihistamine premedication.
Adverse Reactions to Cyclooxygenase Inhibitors (COX-I) in the General Population
| Type of reaction | Clinical presentation | Associated conditions | Hypersensitivity to another COX-I, % | Reaction to other COX-I | Desensitization |
|---|---|---|---|---|---|
| I | Exacerbated respiratory disease | History of nasal polyps, sinusitis, or asthma | 10 | Generally yes | Possible without incident |
| II | Urticaria/angioedema | Chronic urticaria | 30 | Yes, in the activation phase | Effective in 2/3 of patients |
| III | Urticaria/angioedema | No chronic urticaria | 0.3 | Generally yes | Possible without incident |
| IV | Urticaria/angioedema/ anaphalaxis | IgE-mediated | No convincing case reported for aspirin | No; reaction to a specific COX-I | Possible without incident |
| V | Stevens-Johnson syndrome Toxic epidermal necrolysis Pneumonitis | Delayed reactions | < 0.1 | Infrequent | Risk of a new reaction |
COX, cyclooxygenase; IgE, immunoglobulin E.
Prospective patient data were collected between June 2014 and December 2015. In this period, 2402 patients at our center underwent coronary angiography and definitive percutaneous coronary intervention (PCI). Of these patients, 12 (0.5%) showed clear signs of aspirin hypersensitivity and indication for dual antiplatelet therapy. Baseline patient characteristics are presented in Table 2. The mean age was 71.9 years (range, 48-90 years), and 58% of patients were men. The most frequent reaction to aspirin was urticaria and more than half the patients reported previous reactions to other COX inhibitors. In total, 10 patients (83.3%) had acute coronary artery disease, 2 of whom (16.6% of the total) had ST-segment elevation acute coronary syndrome, requiring emergency initiation of the aspirin desensitization protocol. In both patients, possible aspirin hypersensitivity was first noted by the emergency services and confirmed by a rapid patient interview on admission. Desensitization aspirin doses were prepared in advance, and the protocol was begun in the catheterization laboratory and continued in the coronary care unit, thus avoiding any delay in catheterization. Stents were placed in 9 patients, who were therefore maintained on long-term antiplatelet therapy with aspirin and a P2Y12 inhibitor. Desensitization was successful in all patients. Follow-up was conducted through visits, telephone interviews, and review of computerized clinical histories over a mean period of 10.4 months (range, 2-20 months), during which all patients had tolerated the 100mg aspirin dose. None of the patients died during follow-up or showed signs of unstable coronary artery disease.
Patient Characteristics
| Patient | Age, y | Sex | Reaction to apirin | Reaction to another COX inhibitor | Diagnosis | Procedure |
|---|---|---|---|---|---|---|
| 1 | 82 | Male | No recollection | No recollection | Unstable angina | Medical treatment (diffuse coronary disease) |
| 2 | 66 | Male | Urticaria Angioedema | Diclofenac | Non Q AMI | 2 conventional stents (AD and RC) |
| 3 | 80 | Female | Angioedema | Yes. Tolerates paracetamol | Stable angina | 2 pharmacoactive stents (AD) |
| 4 | 77 | Female | Urticaria | Yes. Tolerates meloxicam | Non Q AMI | Coronary surgery |
| 5 | 87 | Female | No recollection | No recollection | Non Q AMI | 1 conventional stent (AD) |
| 6 | 49 | Male | Urticaria | Diclofenac | STEACS | Thrombus aspiration. Complicated plaque in the RI without significant stenosis |
| 7 | 79 | Female | Urticaria | Yes. Tolerates meloxicam | Stable angina | 6 pharmacoactive stents (AD, Cx, and RC) |
| 8 | 90 | Male | Exacerbated asthma | Pyrazolones | STEACS | 1 conventional stent (AD) |
| 9 | 73 | Female | No recollection | No recollection | Unstable angina | 1 pharmacoactive stent (RC) |
| 10 | 63 | Male | Urticaria | Pyrazolones | VF, Non Q AMI | 4 pharmacoactive stents (AD, Cx, and RC) |
| 11 | 48 | Male | Urticaria Angioedema | No recollection | Unstable angina | 1 pharmacoactive stent (AD) |
| 12 | 69 | Male | Angioedema | Possibly paracetamol | Non Q AMI | 1 pharmacoactive stent (Cx) |
AD, anterior descending artery; COX, cyclooxygenase; Cx, circumflex artery; Non Q AMI, non Q-wave acute myocardial infarction; RC, right coronary artery; RI, ramus intermedius artery; STEACS, ST-segment elevation acute coronary syndrome; VF, ventricular fibrillation.
The limitations of this study include the low number of patients, which is also a feature of other published series. In the current study, the small sample size was in part due to the admission interviews conducted by the Allergy Service staff; in several instances, these interviews indicated that there was no aspirin hypersensitivity. Another limitation is that some patients did not recall their previous symptoms with aspirin or other COX inhibitors, and there was therefore uncertainty about what type of reaction to aspirin they had experienced.
In most centers that practice aspirin desensitization, the protocol is initiated 72hours after PCI in patients with ST-segment elevation acute coronary syndrome. In contrast, at our center we practice early desensitization in order to minimize the risk of stent thrombosis. Another notable feature of our protocol is the close involvement of the Allergy Service, whose contribution is central to protocol development, training in admission interviews, evaluation of whether or not to perform the protocol (especially important in patients with uncertain aspirin hypersensitivity), and the prediction and treatment of complications.
The success of centers that carry out aspirin desensitization shows that aspirin hypersensitivity does not necessitate alterations to the therapeutic approach in patients needing dual antiplatelet therapy, including those requiring urgent PCI. Close cooperation with Allergy Service personnel is advisable because their expertise can improve the diagnosis and treatment of aspirin hypersensitivity.
Allergy Service, Hospital de Cabueñes, Gijón, Asturias, Spain.