We present the case of a 49-year-old man with left posterior accessory pathway (AP) pre-excitation in a resting electrocardiogram (ECG) recorded in 2005. He was asymptomatic at the time. A screening electrophysiological study (EPS), without arrhythmogenic drugs, conducted because the patients was a sports player, showed anterograde block of the pathway at 750 ms and absence of retrograde conduction. The refractory period of the pathway was 680 ms with isoproterenol at 2μg/kg/min. After the atrioventricular node reached the Wenckebach block (340 ms), atrial fibrillation (AF) was provoked, with a heart rate of 130 bpm and no pre-excitation observed. Electric cardioversion was required after persistence of AF for 15 minutes (the recordings are not available). The pathway was considered low risk and clinical follow-up was decided.
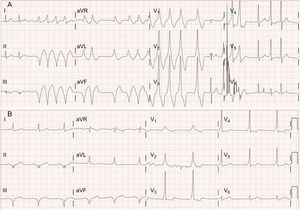
The patient was asymptomatic until 2015, when he attended the clinic for palpitations and presyncope. Atrial fibrillation with pre-excitation was observed with a shorter pre-excited RR interval of 230 ms (Figure 1A). After administration of an amiodarone bolus, the patient reverted to sinus rhythm with constant pre-excitation (Figure 1B). The findings of the EPS were once again low risk, with intermittent pre-excitation at baseline (Figure 2A), anterograde block of the pathway at 580 ms (Figure 2B) and retrograde conduction, and no changes with isoproterenol. In view of the patient's medical history, AP ablation was performed with no complications.
Intracavitary recording during electrophysiology study. DI, DIII, and V1 leads of electrocardiogram, distal (His 1-2) and proximal (His 3-4) His bundle electrocardiogram, electrocardiograms from distal coronary sinus (SC 1-2 in the figure) to proximal coronary sinus (SC 9-10 in the figure). A: Intracavitary recordings showing intermittent pre-excitation (HV interval of 44 ms compared with HV interval of 0 ms). B: Intracavitary recordings during progressive stimulation from the distal coronary sinus to 580 and 570 ms. The first 2 beats show pre-excitation in the left posterior pathway and the third beat with the same coupling cycle shows sudden loss of pre-excitation. From this moment, intermittent pre-excitation is present.
The prevalence of pre-excitation in the general population is 0.1% to 0.3%, although it is asymptomatic in 45% to 60% of these individuals. An association has been found with sudden death resulting from ventricular fibrillation caused by rapid conduction of AF via the AP. The incidence of sudden death ranges from 4.5 episodes per 1000/patients/y of follow-up in symptomatic patients to 3.3 episodes per 10 000 patients/y in asymptomatic patients.1 The latter incidence is very low, but it can be a major cause for concern because it is the first manifestation of the condition.
The clinical guidelines recommend ablation in symptomatic patients, but there is more debate about the management of asymptomatic patients. The 2003 guidelines suggest no treatment as a class I recommendation and catheter ablation as a class IIa recommendation, on the basis of the positive predictive value of EPS and the risk of complications. The 2015 guidelines2 recommend noninvasive tests (exercise testing or Holter ECG studies, as class I recommendations) and EPS (class IIa recommendation). These tests define AP as low or high risk of arrhythmic episodes according to induction of arrhythmias, anterograde conduction capacity, or the presence of RR < 250 ms in AF. Electrophysiological study is highly sensitive but has a low specificity for sudden death given the low incidence of this condition. Moreover, noninvasive studies have been correlated with EPS properties, but these have not been validated in prospective studies of sudden death. This represents a further limitation despite the recommendations of the guidelines. Ablation is recommended in high-risk patients because it reduces the incidence of future arrhythmias and almost completely eliminates the risk of sudden death. The term AP with electrophysiological characteristics of risk has led to misunderstandings when taken as a synonym of risk of sudden death because in most cases this term referred to risk of nonfatal arrhythmias.
The possibility of changes in the conduction properties of APs had already been described in the 1980s with both the worsening (loss of anterograde conduction in 26%-40% of patients) and improvement of conduction (intermittent pre-excitation at baseline with rapid conduction in AF with an RR interval < 250 ms).3 There have been reports of sudden death with apparently low-risk pathways.
In our series (1999-2000), EPS was requested for 580 patients for pre-excitation (553 underwent ablation and 28 did not as the findings in these latter patients were considered low risk and noninducible). All patients remained asymptomatic, apart from the one mentioned above.
In summary, we present a case of low-risk AP (intermittent pre-excitation, limited conduction, and with no conduction during AF) that years later had a transient change in conduction properties which could not be reproduced in EPS despite the administration of isoproterenol (possibly because of the different adrenergic state). The case raises the possibility of considering ablation during baseline EPS in all cases due to the risk of conversion in the future. Currently, we have no information on the risk of conversion or the consequences. It is therefore recommended to tailor management to individual cases and assess the option of initial direct ablation depending on the site, vascular access, experience of the operators, and the patient preferences.4