Ischemic stroke is a disabling disease and its association with pregnancy and puerperium is uncommon.
A 32-year-old woman was admitted to the emergency room with acute neurologic symptoms including left hemiparesis, dysarthria, and chorea, 2 months after cesarean surgery for severe pre-eclampsia. Relevant medical history included a spontaneous abortion 5 years previously, intermittent gingival bleeding during pregnancy and leukocytosis during hospitalization for the caesarian surgery.
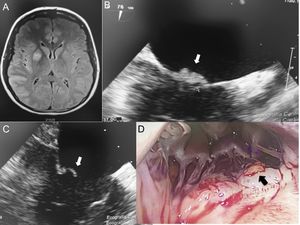
Initial workup including a cerebral scan, showed images of acute ischemic insult in the right parietal, temporal, and frontal lobes (Figure 1A). The results of electrocardiogram and complete blood count were normal.
A: cerebral magnetic resonance imaging: acute ischemic images in the middle cerebral artery territory. B,C: transesophageal echocardiography, showing a 6-mm mobile mass on the atrial side of the mitral valve (white arrow). D: thoracotomy view showing a yellow mass on the atrial side of the mitral valve (black arrow).
Due to the localization of stroke, a cardiovascular consultation was requested. The carotid and transcranial Doppler were normal. Transoesophageal echocardiography showed multiple small (6mm) mobile vegetations in the atrial side of the mitral valve (Figure 1B, C). Blood cultures were negative for bacterial or fungi. C-reactive protein and procalcitonin were within normal limits.
The patient regained complete neurological function 2 days after initial presentation with no sequelae. After exclusion of common etiologies for cardiac vegetations including bacteremia, a comprehensive workup was carried out to exclude autoimmune and neoplastic processes. The rheumatologic panel was negative for antiphospholipid syndrome, lupus and other autoimmune diseases. No evidence of thrombophilia or blood dyscrasias were identified. A missense mutation (C677T) of the methylenetetrahydrofolate reductase (MTFHR) gene was detected without hyperhomocysteinemia. A full body positron emission tomography-scan as well as serum concentration of CA125 and CA15-3 were negative.
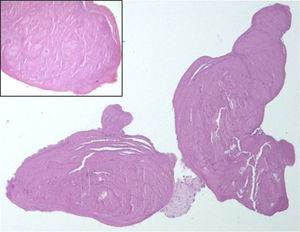
At day 8, a follow-up cerebral scan showed a new ischemic image in the right parietal lobe (not shown), which prompted cardiac surgery via mini thoracotomy. Six “brain-like” masses of less than 1mm, adhering to the atrial side of both leaflets of the mitral valve, were identified (Figure 1D). They were carefully resected with preservation of the valve. Culture of the masses was negative for microorganisms. Histologic examination of the specimen showed features compatible with nonbacterial thrombotic endocarditis (NBTE) (Figure 2).
The patient had a favorable, uncomplicated postsurgical course and was discharged 7 days after surgery without neurological sequelae and under oral anticoagulant therapy. At the 12 month follow-up, she is still asymptomatic with oral anticoagulation and with no mitral masses identified in subsequent transoesophageal echocardiography.
Nonbacterial thrombotic endocarditis is a disease characterized by endocardial vegetations primarily composed of a sterile matrix of platelets and fibrin that deposits on cardiac valves.1 Nonbacterial thrombotic endocarditis is most commonly associated with neoplastic diseases, long-term illnesses, sepsis, and burns. While NBTE can be asymptomatic, up to 42% of patients can present with embolic events, especially affecting the cerebral arterial tree.2 Other conditions, such as hyperhomocysteinemia due to mutations of the MTHFR gene, are a common cause of inherited prothrombotic states that can be associated with NBTE.3
Clinical diagnosis of NBTE is challenging and requires a high level of suspicion. Anticoagulation due to alterations in patients’ coagulation status has been recommended by some authors.4
In our case, after excluding other etiologies, the increased clotting tendency of the patient during pregnancy and puerperium (also related to the appearance of preeclampsia) was thought to be the cause of NBTE. There are few cases in the literature that support this association and in those cases the diagnosis was conducted postmortem.5 The detection of the MTHFR gene mutation is also important because it could be another factor increasing the risk of hypercoagulability in our patient, even when the values of homocysteinemia were normal (maybe due to diet).
Echocardiographic techniques such as transesophageal echocardiography have higher sensitivity (90%) for the diagnosis of intracardiac vegetations but a distinction between NBTE and infective endocarditis is not feasible. Furthermore, no clear morphological features of the NBTE vegetations assessed by imaging can predict embolic risk.6
To our knowledge, there are no guidelines for surgical intervention in patients with NBTE, but surgery has been recommended in patients presenting with acute cardiac failure and recurrent thromboembolism despite anticoagulation.6
.