The natural history of heart failure (HF) is marked by decompensations, which usually require hospitalization. In Spain, the number of hospital admissions for HF has increased in recent decades.1,2 In addition to the inherent cost, in-hospital mortality is also high.3 Prevention of readmission should therefore be one of the main objectives of the treatment of outpatients with HF. Most models for predicting readmission are based on data from hospitalized patients and so they do not reliably reflect the clinical condition of outpatients. Recently, our group has developed a new tool, the Redin-SCORE,4 to calculate the risk of readmission due to HF in the short- and long-term for outpatients. The score is easy to calculate and uses 6 parameters regularly monitored in patients with HF: presence of signs of left HF (paroxysmal nocturnal dyspnea, orthopnea, third heart sounds or crackles); heart rate > 70 bpm; anemia (hemoglobin < 130g/L in men and < 120g/L in women); N-terminal fraction of brain natriuretic peptide > 1000 ng/L; glomerular filtration rate < 60mL/min/1.73 m2; and dilated left atrium in the echocardiogram (> 26 mm/m2). However, one of the limitations inherent in any score is the need of validation in other populations and, in our particular case, the low incidence of events (17%) recorded in the original sample. Therefore, to extend the validity of this new risk scale, it was decided to assess its predictive and discriminatory capacity in a contemporary cohort of outpatients with heart failure.
To this end, a prospective study was undertaken with patients referred for the first time to the HF unit of our hospital between June 2012 and December 2014 (n=237). Follow-up was performed by a trained group of cardiologists and nursing staff through review of medical records and telephone calls to register data on hospitalization for HF during the following year. The discriminatory capacity was calculated using the C statistic. The calibration, slope, and intersection of the model were assessed using the Hosmer-Lemeshow goodness-of-fit test. The decision curves were analyzed to determine when application of the Redin-SCORE increased the number of true positives without increasing the number of false negatives.5,6
Of the 237 patients included, 5.4% (13 patients) required admission for HF during the first month and 29.5% (70 patients) during the first year. The main characteristics of the cohort according to the presence of events at follow-up are shown in the Table. The patients who were admitted for HF were older and a higher proportion had ischemic heart disease. They were also in a more advanced functional class. In the laboratory tests, these patients had a lower glomerular filtration rate and more frequently had anemia and elevated N-terminal fraction of brain natriuretic peptide. Mortality and need for heart transplant were also higher in these patients.
Baseline Characteristics of the Population According to Risk of Heart Failure at 1 Year
| No admission (n = 167) | Admission for HF (n = 70) | P | |
|---|---|---|---|
| Men | 114 (68) | 50 (71) | .630 |
| Age, y | 65 ± 14 | 70 ± 11 | .008 |
| Atrial fibrillation | 60 (36) | 29 (41) | .425 |
| Ischemic origin | 44 (26) | 32 (46) | .004 |
| Diabetes mellitus | 53 (32) | 30 (43) | .102 |
| Hypertension | 118 (71) | 55 (79) | .211 |
| Dyslipidemia | 73 (44) | 46 (66) | .002 |
| History of smoking | 115 (69) | 44 (63) | .369 |
| NYHA III-IV | 53 (32) | 46 (66) | <.001 |
| COPD | 40 (27) | 20 (31) | .557 |
| SBP, mmHg | 126 ± 21 | 120 ± 22 | .085 |
| LVEF, % | 40 ± 17 | 41 ± 18 | .651 |
| NT-proBNP, ng/L | 2.968 ± 5.481 | 6.143 ± 7.679 | .002 |
| GFR (CKD-EPI, mL/min/1.73 m2 | 62 ± 20 | 53 ± 19 | .001 |
| Hemoglobin, g/L | 134 ± 18 | 126 ± 18 | .002 |
| β-blockers | 146 (87) | 56 (80) | .142 |
| ACEI/ARA-II | 147 (88) | 60 (86) | .626 |
| Furosemide | 129 (77) | 65 (93) | .004 |
| Aldosterone antagonists | 75 (45) | 38 (54) | .187 |
| Pacemaker | 19 (13) | 15 (23) | .057 |
| Resynchronization | 13 (8) | 8 (11) | .368 |
| ICD | 29 (17) | 14 (20) | .631 |
| Heart transplant | 3 (2) | 5 (7) | .038 |
| Signs of left HF | 25 (15) | 22 (31) | .004 |
| HR > 70 bpm | 89 (53) | 37 (53) | .951 |
| Anemia | 51 (31) | 36 (51) | .002 |
| NT-proBNP > 1000 ng/L | 94 (56) | 58 (83) | <.001 |
| GFR < 60 mL/min/1.73 m2 | 60 (36) | 44 (63) | <.001 |
| LA > 26 mm/m2 | 77 (46) | 44 (63) | .019 |
| Overall mortality, % | 4 (2) | 22 (31) | < .001 |
| Discrimination and calibration in the overall population | C statistic | P value: Hosmer-Lemershow | Slope | Intersection |
|---|---|---|---|---|
| Readmission for HF at 1 mo | 0.67 | .458 | 0.54 | −1.23 |
| Readmission for HF at 1 y | 0.71 | .601 | 1.05 | 0.05 |
ACEI, angiotensin converting enzyme inhibitor; ARA-II, angiotensin II receptor antagonist; CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; COPD, chronic obstructive pulmonary disease; GFR, glomerular filtration rate; HF, heart failure; HR, heart rate; ICD, implantable cardioverter device; LA, left atrium; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association functional class; SBP, systolic blood pressure.
Data are expressed as No. (%) or mean ± standard deviation.
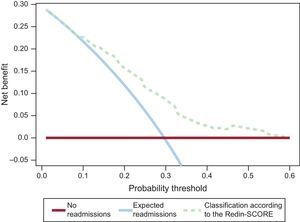
The analysis of risk categories according to the Redin-SCORE obtained showed a progressive increase in the percentage of events, both at 1 month (< 20 points, 3.2%; ≥ 20 points, 9.4%; P = .04) and at 1 year (≤ 12 points, 12.2%; 13–20 points, 36%; 21–30 points, 47%; P < .001). Given the difference in recorded events between the derived population and the external validation population, the probabilities of different scores were recalibrated and nonsignificant values were obtained in the goodness-of-fit test (Table). In addition, the C statistics in the current cohort were not significantly different from the discrimination measures generated in our original series (C = 0.67 vs C = 0.73 at 1 month, P = .459; C = 0.71 vs C = 0.67 at 1 year, P = .295). In the external validation performed previously in the MUSIC cohort, values for a C index of 0.71 and 0.69 were obtained at 6 months and 1 year, respectively. The Figure shows the decision curves analysis, which shows that application of the Redin-SCORE improves the net benefit with respect to the strategy of not applying any discrimination to the population of patients with HF.
Decision curves for the Redin-SCORE model for predicting readmission for HF at 1 year. The x axis represents the probability threshold for readmission for HF according to the Redin-SCORE. The y axis represents the net benefit ([true positives - w x false positives] / total number of patients): positive values indicate an improvement in the classification of patients, and w is a correction factor for the probability threshold. The upper limit is 0.30 because the incidence of readmission for HF in study was 30%. The continuous red line indicates that no patient was readmitted for HF at 1 year. The blue line assumes that all expected patients were readmitted, 30% during the first year. The dotted line represents the result of applying the Redin-SCORE model. Thus, for a probability of readmission at 1 year of between 10% and 60%, the Redin-SCORE provides a net benefit due to better classification of the patients. HF, heart failure.
The present study provides external validation for the Redin-SCORE, a new scale for predicting short- and long-term readmission for HF in outpatients. In a contemporary cohort of patients with HF, the Redin-SCORE showed acceptable discriminatory capacity and calibration, particularly at 1 year. This study supports its clinical usefulness as a stratification tool for patients with HF in Spain.
FUNDINGCooperative Health Research Thematic Networks of the Carlos III Health Institute (REDINSCOR) [no. RD06-0003-0000] and Cardiovascular Research Network of the Carlos III Health Institute (RIC) [no. RD12/0042/0002].

![Decision curves for the Redin-SCORE model for predicting readmission for HF at 1 year. The x axis represents the probability threshold for readmission for HF according to the Redin-SCORE. The y axis represents the net benefit ([true positives - w x false positives] / total number of patients): positive values indicate an improvement in the classification of patients, and w is a correction factor for the probability threshold. The upper limit is 0.30 because the incidence of readmission for HF in study was 30%. The continuous red line indicates that no patient was readmitted for HF at 1 year. The blue line assumes that all expected patients were readmitted, 30% during the first year. The dotted line represents the result of applying the Redin-SCORE model. Thus, for a probability of readmission at 1 year of between 10% and 60%, the Redin-SCORE provides a net benefit due to better classification of the patients. HF, heart failure. Decision curves for the Redin-SCORE model for predicting readmission for HF at 1 year. The x axis represents the probability threshold for readmission for HF according to the Redin-SCORE. The y axis represents the net benefit ([true positives - w x false positives] / total number of patients): positive values indicate an improvement in the classification of patients, and w is a correction factor for the probability threshold. The upper limit is 0.30 because the incidence of readmission for HF in study was 30%. The continuous red line indicates that no patient was readmitted for HF at 1 year. The blue line assumes that all expected patients were readmitted, 30% during the first year. The dotted line represents the result of applying the Redin-SCORE model. Thus, for a probability of readmission at 1 year of between 10% and 60%, the Redin-SCORE provides a net benefit due to better classification of the patients. HF, heart failure.](https://static.elsevier.es/multimedia/18855857/0000006900000012/v5_201710091326/S1885585716302109/v5_201710091326/en/main.assets/thumbnail/gr1.jpeg?xkr=eyJpdiI6ImlrYU1WUTMwNmNvMCtVWVROQ1ZCWFE9PSIsInZhbHVlIjoiQlZyMVFXekEzQ3dOY2cyUm9VSmpxMDc0WlY3eVlCbnprVG1Md3ExYStLST0iLCJtYWMiOiI1ZGU5MmFhMDM1NzY0ODcyZDhhZGE1MjFmMWNlNGEyOTMwMGFjMmY4NGU2YzQxYzMzMTM0MWQxNWU1N2VmNWMwIiwidGFnIjoiIn0=)