Keywords
INTRODUCTION
Numerous studies support the use of brain natriuretic peptide, also known as B-type natriuretic peptide (BNP), as a risk marker in various cardiovascular conditions; however, the predictive value attributable to BNP in an unselected population admitted for acute heart failure (AHF) remains uncertain, and its influence on intermediate episodes, such as new hospital readmissions assessed independently (not as part of a combined event), has still not been described. The aim of our study was to assess the relationship between BNP, measured during the AHF episode, and mortality and hospital readmission for AHF, adjusting for mortality as a competing event.
METHODS
Study Group and Protocol
We prospectively included 569 patients admitted to the cardiology department of our hospital with a diagnosis of AHF between June 1, 2004 and December 31, 2006. The diagnosis was established by cardiologists in accordance with the current recommendations.1 Patients with acute coronary syndrome, active neoplastic or infectious disease, or end-stage renal disease on dialysis were excluded from the study, as were patients who were initially admitted with AHF but whose main reason for admission was considered to be other than AHF (n=32). The patients were individually managed, following current recommendations.1 During admission, a single observer performed the transthoracic echocardiography. BNP (as measured by the ADVIA Centaur immunoassay system) was determined within a median of 48 hours (range, 42-54 h) after hospital admission and always after the first 24 hours.
Statistical Analysis
Continuous variables were expressed as mean (SD) or median (interquartile range) as appropriate, and discrete variables as percentages. The baseline characteristics of the population were stratified by BNP distribution quintile. Analysis of variance was used to compare continuous variables with normal distribution; otherwise, the Kruskal-Wallis test was used. For discrete variables, the c2 test was used. The linear trend of proportions was also analyzed using the linear trend test. The percentage of deaths in each BNP category was estimated by Kaplan-Meier curves, and the differences were quantitated by the log-rank test. The adjusted proportion of readmissions for AHF was estimated by cumulative incidence, and the differences between BNP quintiles were quantitated by the Gray test.2 To assess the intrinsic effect of BNP on the hospital readmission rate, contingent on whether the patient was living during follow-up, the conditional probability method of Pepe et al3 was used. The Cox regression model was used to analyze the association between BNP and mortality, whereas the regression model of Fine et al4 and Gray2 was used for competing risks of readmission due to AHF. In both cases, or if the variable presented P<.2 in the univariate analysis, variables of recognized prognostic value in the medical literature were included. Once the initial models had been established, they were simplified by stepdown elimination. The estimated coefficients were expressed as the hazard ratio (HR) with the respective 95% confidence intervals (CI). The final discriminatory ability of the multivariate models was determined by Harrell's C statistic. A P value less than .05 was considered significant in all cases. The STATA 9.2 and R (cmprsk) statistical packages were used for the statistical analyses.
RESULTS
Sample Characteristics Stratified by BNP Level
The mean age (SD) of our population was 73.8 (10.6) years; 52.4% were women. The mean (SD) and the median BNP level were 311 (425) and 152 (interquartile range, 90-356) pg/mL, respectively. In general, a positive, monotonic association was observed between the most common AHF severity parameters and the BNP quintiles (Table 1).
Relationship of BNP With Mortality
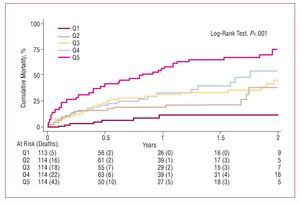
During a median follow-up of 9 (interquartile range, 3-18) months, 156 (27.4%) deaths were recorded, 24 for the index hospitalization and 132 after hospital discharge. The mortality distribution stratified according to BNP quintile showed a monotonic increase from lowest to highest BNP quintile (6.1%, 20.2%, 26.3%, 29.8%, and 54.9%; trend, P<.001) (Figure 1). In the final multivariate analysis, BNP was positively and closely associated with mortality (Table 2). We did not include variables such as left ventricular ejection fraction, type of AHF, or ischemic etiology in the final model, due to the absence of statistical association with mortality. Additionally, no significant interactions were found between BNP levels and potential confounding variables such as left ventricular systolic function, etiology of heart failure, kidney function, or gender. The Harrell's C statistic was higher in the model that included BNP compared to the same model without this value (0.801 vs 0.781).
Figure 1. All-cause mortality during follow-up, stratified by BNP quintile. The number of patients at risk and the number of deaths that have occurred are specified at each follow-up point. BNP indicates brain natriuretic peptide.
Relationship of BNP With Hospital Readmissions for AHF
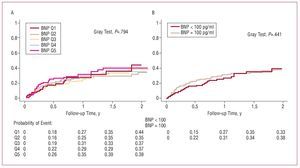
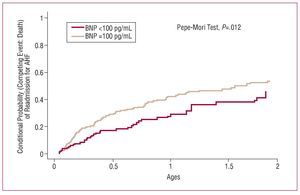
During follow-up, 140 (24.6%) hospital readmissions for AHF were recorded. The percentages of readmissions corresponding to the BNP quintiles were, from lowest to highest, 21.1%, 21.9%, 22.8%, 26.3%, and 31% (trend, P=.058). Figure 2 shows the curve of hospital readmissions, stratified by BNP quintile or by BNP ≥100 pg/mL. BNP did not show a significant effect in either case (Gray test, P=.79 and P=.44, respectively). To estimate the theoretical effect that BNP might have on the hospital readmission rate for AHF in the ideal context where mortality as a competing event could be eliminated, we decided to use the conditioned probability model.4 Figure 3 shows a significant separation between dichotomized BNP levels (≥100 pg/mL), which confirmed its innate predictive value for readmission due to AHF, even though the high simultaneous mortality rate in our population masked this property.
Figure 2. A: cumulative incidence of readmissions, stratified by BNP quintiles. B: cumulative incidence of readmissions stratified by BNP level, dichotomized according to 3100 pg/mL and <100 pg/mL. Both cases were adjusted for mortality during follow-up as a competing event. Abbreviations: BNP, brain natriuretic peptide.
DISCUSSION
In this study on a consecutive population of patients admitted with a diagnosis of AHF, we found a positive, strong, and independent association between BNP levels (measured during the first few days of hospitalization) and mortality. In addition, the analysis of intermediate events, examined with the use of innovative methodology, showed that BNP levels were not associated with a risk of hospital readmission due to AHF; however, this finding was influenced by the high mortality rate of our population, which prevented BNP from showing its biological value as a predictive factor for readmissions.
Optimal Time Point for BNP Measurements
Because BNP has a short half-life (15-20 min), the variation observed in baseline values following the administration of aggressive treatment is substantial. This fact, rather than a problem, has been used as a clinical tool to assess therapeutic response; thus, most studies that analyze the prognostic value of BNP or NT-proBNP after an AHF event report that serial or pre-hospital discharge measurements are prognostically superior to measurements taken at admission. However, this approach limits in-hospital prognostic stratification and BNP cannot be used as a therapeutic guide, as several other studies have indicated. Our approach, which consisted of measuring BNP after initial clinical stabilization, provides a biologically feasible strategy, integrating information from BNP levels at admission and its theoretical response after initial aggressive treatment, making it possible to perform risk stratification earlier than when BNP is measured before hospital discharge.
BNP and Hospital Readmissions for AHF
BNP, in any of its presentations, showed no predictive value for readmission due to AHF (Figure 2). However, the conditional probability analysis confirmed that, under ideal and theoretical circumstances in which mortality could be eliminated, BNP has significant predictive effect for hospital readmission due to AHF (Figure 3).
Figure 3. Conditional probability of readmission for acute heart failure (AHF), eliminating death as a competing event, stratified by BNP level into 3100 pg/mL and <100 pg/mL. BNP indicates brain natriuretic peptide.
Limitations
This study has certain limitations. First, its observational nature may have introduced bias related to the difficulty for including prognostic variables that are unknown or not collected in our records. Second, although BNP was usually measured early in the hospitalization, it was not done in all patients at the same time point after admission, a fact that introduces some variability. Lastly, owing to the absence of serial measurements, we cannot establish the time point offering the greatest prognostic yield in this situation.
This study received a grant from Siemens Medical Solutions Diagnostic SL.
Correspondence: Dr J. Núñez Villota.
Servicio de Cardiología. Hospital Clínic i Universitari. Avda. Blasco Ibáñez, 17. 46010 Valencia. España.
E-mail: yulnunez@gmail.com
Received August 17, 2007.
Accepted for publication February 1, 2008.