Keywords
Received March 11, 2005. Accepted for publication May 10, 2005.
INTRODUCTION
Obesity is an important risk factor for postoperative complications following heart surgery and significantly increases the incidence of in-hospital infections and mortality. Percutaneous treatment of concomitant valve disease and coronary disease may be an effective, less aggressive alternative with potentially fewer complications among high-risk surgical patients.
CASE STUDY
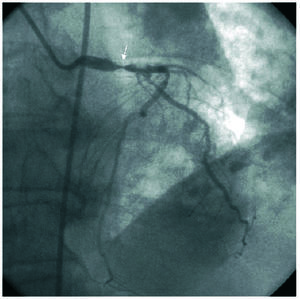
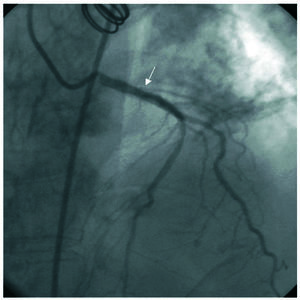
A 65-year-old woman with a body mass index of 44 and a history of hypertension, type 2 diabetes, right lobectomy due to childhood tuberculosis with moderate pulmonary restriction, and Graves-Basedow disease was admitted for surgery for morbid obesity. During the hospitalization, she was assessed by the cardiology department for an episode of chest pain that lasted 30 minutes. Cardiopulmonary auscultation revealed an aortic ejection murmur and hypoventilation in both lung fields; the electrocardiogram showed sinus rhythm with no evidence of acute ischemia. The blood analyses indicated elevation of myocardial lesion markers (troponin I, 8 ng/dL and creatine kinase, normal); hence, coronary angiography was performed. The diagnostic catheterization disclosed a severe calcified lesion of the left main stem that encompassed the origin of the circumflex artery and a 50% lesion in the middle segment of the left anterior descending artery (Figure 1). Ventriculography showed normal overall ventricular function with no regional contractility alterations. Measurement of the left ventricular and aortic pressures gave a peak-to-peak gradient of 100 mm Hg and average of 60 mm Hg. Based on these findings, the patient was considered ineligible for bariatric surgery and at high risk for heart surgery due to obesity; therefore, conservative medical treatment was initiated. Two months later the patient was readmitted to the coronary unit for acute pulmonary edema secondary to atrial fibrillation with rapid ventricular response and discharged following stabilization and medical treatment. Two months later she was again admitted with a diagnosis of Killip Class III acute myocardial infarction; palliative percutaneous treatment was decided because of the patient's poor progress. Aortic valvuloplasty was performed using a Cribier Laetac® balloon and the peak-to-peak gradient dropped from 100 to 40 mm Hg. A paclitaxel-coated stent (Taxus 3.5×12 mm) was implanted in the left coronary trunk during the same procedure, along with another stent in the ostium of the circumflex artery (Taxus 2.75×16 mm) (Figure 2). Four months later the patient was cardiologically stable and asymptomatic, and was able to undergo bariatric surgery consisting of gastrectomy, cholecystectomy, and biliopancreatic diversion, with an uneventful postoperative period. Eight months later she was admitted for chest pain. Diagnostic catheterization was repeated showing absence of in-stent restenosis; however, there was a 60% lesion in the middle segment of the left anterior descending artery was seen. The mean aortic transvalvular gradient was 50 mm Hg. By that time, the patient had lost 30% of her body weight and the body mass index was 31; therefore, she was accepted by the cardiac surgery department. On-pump aortic valve replacement with a 21 Omnicarbon prosthesis and an internal mammary artery bypass to the left anterior descending artery were performed. The postoperative was uneventful, and the patient remained asymptomatic one year later.
Figure 1. Left anterior oblique view showing a calcified lesion in the left coronary trunk that encompasses the origin of the circumflex artery.
Figure 2. Angiographic image following stent placement in the left coronary trunk and in the ostium of the circumflex artery.
DISCUSSION
Obesity raises the risk of any type of surgery, significantly increasing the risk of infections and in-hospital mortality. Morbid obesity is defined as a body mass index ≥40. In these patients, diet and behavioral therapies fail in 90% of the cases. Surgical treatment is more successful and in most cases achieves a reduction of 50% in preoperative weight, thus lowering the risks associated with severe obesity.1
Combined aortic valve replacement and coronary revascularization surgery was indicated in our patient. However, the surgical risk calculated by the EuroSCORE2 was extremely high and conservative treatment was initially decided. Given the patient's poor clinical progress, percutaneous treatment of both the aortic stenosis and the coronary lesions was chosen as an alternative with the aim of performing bariatric surgery followed by heart surgery sometime later.
Aortic valvuloplasty can be used as palliative treatment for patients with symptomatic aortic stenosis when valve replacement surgery is contraindicated. This therapeutic alternative has been used in elderly patients and in patients in cardiogenic shock as a bridge to subsequent heart surgery. Ten percent of cases develop severe complications, and restenosis appears in most patients within 6-12 months after valvuloplasty.3,4
Additionally, a significant lesion in the left main stem is an indication for surgical revascularization. The high associated risk and the high incidence of restenosis with conventional stents have been some of the arguments used against percutaneous surgery for lesions in this location. The incidence of restenosis is considerably lower with the use of drug-coated stents, making percutaneous management of these lesions a safe alternative for some patients.5,6
The literature review revealed only a few cases of aortic valvuloplasty combined with coronary angioplasty in older patients and in patients with cardiogenic shock.7 This is the first time this treatment has been described as an alternative for a patient with morbid obesity and at high surgical risk.
Correspondence: Dra. L. Salido Tahoces.
Hospital Ramón y Cajal.
Ctra. de Colmenar, km 9,100. 28039 Madrid. España.
E-mail: luisasalido@hotmail.com