Obesity is an increasingly prevalent cardiovascular risk factor.1 It implies a hemodynamic overload, leading to functional anatomical changes in the heart, with ventricular hypertrophy and systo-diastolic dysfunction.2
The most effective treatment is bariatric surgery, which has a cardioprotective effect, improving ventricular geometry and function.3
We analyzed medium-term structural and functional changes in the hearts of patients with morbid obesity who had bariatric surgery.
This was a prospective study of patients with morbid obesity followed up in the Obesity Unit and referred for bariatric surgery between January 2010 and June 2014. Patients with coronary artery disease, valve disease, cardiomyopathies, or congenital heart disease were excluded.
Patients had an echocardiogram 1 month before and 6 months after surgery. The assessments were performed by an experienced examiner, who did not know if it was the first or second study.
For the left ventricular (LV) geometry study, M-mode was used to obtain ventricular diameters, wall thickness, and relative wall thickness (RWT):
RWT=(2×posterior wall) / LV end-diastolic diameter
Left ventricular mass was calculated according to the Devereux formula, with height indexed to the power of 2.7 to minimize interference of obesity.4
An LV mass index (LVMI) ≥ 51g/m2.7 constituted hypertrophy. Patients were classified into 4 geometric patterns, according to RWT and LVMI:
- 1.
Normal, RWT < 0.45 and LVMI < 51g/m2.7.
- 2.
Concentric remodeling, RWT ≥ 0.45 and LVMI < 51g/m2.7.
- 3.
Eccentric hypertrophy, RWT < 0.45 and LMVI ≥ 51g/m2.7.
- 4.
Concentric hypertrophy, RWT ≥ 0.45 and LMVI ≥ 51g/m2.7.
Geometric pattern was considered an ordinal qualitative variable, with concentric hypertrophy being the least favorable pattern, followed by eccentric hypertrophy, and concentric remodeling.
Evaluation of LV systolic function was based on ejection fraction from the Teichholz method, and tissue Doppler analysis of systolic mitral annular displacement. Evaluation of LV diastolic function was based on pulsed Doppler of mitral flow and tissue Doppler of diastolic mitral annular displacement. Patients were classified into 3 groups according to diastolic function5: a) normal filling, b) impaired relaxation, and c) pseudonormal filling.
For statistical analysis, the statistics package STATA v. 12.1 was used. Continuous variables were expressed as mean±standard deviation, and categorical variables were expressed as absolute values and percentages. Changes in continuous quantitative variables were analyzed with the paired Student t test, and changes in ordinal qualitative variables were analyzed with the Wilcoxon signed rank test.
Thirty-two patients completed the study. They had a mean age of 45.1 years, and 87.5% were women. Associated comorbidities consisted of hypertension in 56.3%, diabetes in 34.4%, dyslipidemia in 21.9%, and smoking in 28.1%. Mean body mass index before surgery was 47.3.
At 6 months postsurgery, there was a loss of 30.2%±9.2% of baseline body weight, improved metabolic profile, and a reduction in the number of antihypertensive medications (Table). The echocardiographic findings were as follows:
- •
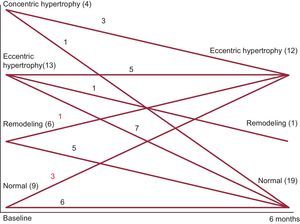
Structural findings: baseline mean LV diameters were normal. Mean RWT was 0.41, and mean LVMI was 50.8kg/m2.7. Baseline geometric pattern: 28.1% of patients had a normal pattern. Of those with abnormal ventricular geometry, more than 50% had hypertrophy, with eccentric hypertrophy being the most common. At 6 months postsurgery, the LV end-diastolic diameter had increased and there was a reduction in wall thickness and RWT. There was no significant change in LVMI. At the end of the study, the geometric pattern showed significant improvement (Figure).
- •
Functional changes: LV systolic function was normal in all patients and did not change. Regarding LV diastolic function, 28% of patients had normal filling, almost 69% had an impaired relaxation pattern, and 3% had pseudonormal filling. At the end of the study, E wave velocity had increased, E/A ratio had decreased, and deceleration time had shortened. At the end of follow-up, LV diastolic function had significantly improved, with 69% of patients showing normal filling.
Patient Clinical and Echocardiographic Characteristics Before and After Surgery (n=32)
| One month before surgery | Six months after surgery | P | |
|---|---|---|---|
| LVMI2.7 | 50.8±14.7 | 49.8±15.8 | .77 |
| Systolic BP, mmHg | 136.17 | 121.17 | .001 |
| Diastolic BP, mmHg | 81.17 | 77.55 | .26 |
| Number of antihypertensive medications | 1.17±0.71 | 0.67±0.6 | .008 |
| HR, bpm | 72.1 | 69.7 | .79 |
| LA diameter, mm | 41.39 | 40.9 | .62 |
| LVEF, % | 68.6±1.4 | 69.1±1.9 | .9 |
| S’ velocity on TDI | 9.4±0.5 | 8.8±0.3 | .1 |
| RWT, mm | 0.4±0.1 | 0.3±0.05 | .03 |
| LVEDD, mm | 49.4±7.4 | 52.8±5.5 | < .01 |
| LVESD, mm | 29.8±5.6 | 31.0±5.1 | .27 |
| Septum, mm | 10.1±1.4 | 8.9±1.4 | < .001 |
| Posterior wall, mm | 9.9±1.6 | 8.9±1.4 | .01 |
| E/A ratio | 0.9±0.3 | 1.3±0.3 | < .001 |
| E/E’ ratio | 8.2±0.34 | 9.4±0.5 | .01 |
| Deceleration time, ms | 230.3±10.1 | 184.8±11.2 | .03 |
| Normal diastolic function, % | 28.1 | 68.8 | .002 |
| Normal geometric pattern | 9 (28.1) | 19 (59.4) | .007 |
| Concentric remodeling | 6 (18.8) | 1 (3.1) | |
| Eccentric hypertrophy | 13 (40.6) | 12 (37.5) | |
| Concentric hypertrophy | 4 (12.5) | 0 |
BP, blood pressure; HR, heart rate; LA, left atrium; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; LVESD, left ventricular end-systolic diameter; LVMI2.7, left ventricular mass index (LV mass in grams, divided by height in meters to the power of 2.7); RWT, relative wall thickness; TDI tissue Doppler imaging.
A high percentage of our patients showed some type of ventricular remodelling, the most common type being eccentric hypertrophy, which concurs with reports by other authors.6 Unlike other studies, the improved geometric pattern in our patients was fundamentally due to a marked reduction in RWT, with no significant changes in LVMI. This improvement in ventricular geometry was accompanied by normalization of diastolic function in more than half of the patients.
.