The prognosis of Marfan syndrome (MS) is principally determined by aortic involvement (especially affecting the aortic root), which is the most common cause of death and reduced life expectancy in MS patients.
The classic standard treatment for aortic root aneurysm is root replacement with a valved conduit (the Bentall procedure); however, the complications inherent in the use of prosthetic valves1 has driven the development of techniques for aortic root replacement that preserve the aortic valve, and aortic valve reimplantation has shown excellent short- and long-term results.2 Nevertheless, the use of this method in MS patients remains controversial due to the small number of cases, the short follow-up, and the uncertain long-term stability and functioning of the repaired aortic root.
We analyzed long-term survival and the rates of reoperation and recurrent aortic regurgitation (AoR) > grade II among MS patients undergoing valve-sparing aortic root repair at our center.
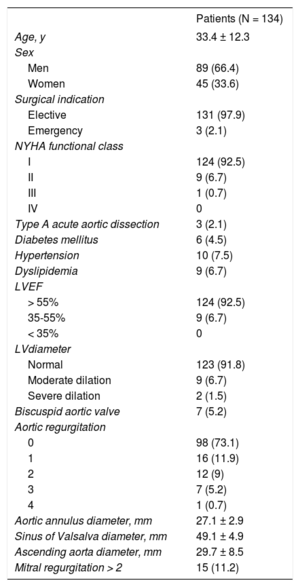
Between March 2004 and June 2018, 134 patients diagnosed with MS according to clinical criteria and genetic analysis underwent aortic valve reimplantation (the David procedure) (Table 1). Surgery was indicated for emergency repair of type A aortic dissection or as an elective intervention in patients with an aortic root diameter ≥ 50mm or ≥ 45mm in the presence of risk factors.1 In 35 patients, aortic valve reimplantation was combined with other aortic repair techniques, and 18.7% of patients also required other cardiac procedures. In-hospital mortality was 0%. Mean follow-up was 6.2 ± 3.9 years, with an annual echocardiography examination and computed tomography or magnetic resonance every 2 years. All patients were periodically assessed at our Marfan unit.
Preoperative Clinical Characteristics and Echocardiography Parameters.
| Patients (N = 134) | |
|---|---|
| Age, y | 33.4 ± 12.3 |
| Sex | |
| Men | 89 (66.4) |
| Women | 45 (33.6) |
| Surgical indication | |
| Elective | 131 (97.9) |
| Emergency | 3 (2.1) |
| NYHA functional class | |
| I | 124 (92.5) |
| II | 9 (6.7) |
| III | 1 (0.7) |
| IV | 0 |
| Type A acute aortic dissection | 3 (2.1) |
| Diabetes mellitus | 6 (4.5) |
| Hypertension | 10 (7.5) |
| Dyslipidemia | 9 (6.7) |
| LVEF | |
| > 55% | 124 (92.5) |
| 35-55% | 9 (6.7) |
| < 35% | 0 |
| LVdiameter | |
| Normal | 123 (91.8) |
| Moderate dilation | 9 (6.7) |
| Severe dilation | 2 (1.5) |
| Biscuspid aortic valve | 7 (5.2) |
| Aortic regurgitation | |
| 0 | 98 (73.1) |
| 1 | 16 (11.9) |
| 2 | 12 (9) |
| 3 | 7 (5.2) |
| 4 | 1 (0.7) |
| Aortic annulus diameter, mm | 27.1 ± 2.9 |
| Sinus of Valsalva diameter, mm | 49.1 ± 4.9 |
| Ascending aorta diameter, mm | 29.7 ± 8.5 |
| Mitral regurgitation > 2 | 15 (11.2) |
LV, left ventricle; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association.
Data are expressed as no. (%) or mean ± standard deviation
Survival at 1 year was 100% and remained high at 5 and 10 years (99% ± 1% and 97.1% ± 2%, respectively) (Figure 1). During follow-up, moderate or severe AoR developed in 7 patients (5.4%), 3 of whom underwent reintervention, mild AoR developed in 9 patients, and AoR was trivial or absent in the rest of the study population. Of 17 patients with a postoperative valve leaflet coaptation height ≤ 7mm, 3 (18%) developed significant AoR (≥ grade II), and poor leaflet coaptation was the only predictor of significant postoperative AoR (hazard ratio [HR], 1.9; P = .02). Freedom from significant AoR at 1, 5, and 10 years postintervention was 99.1% ± 0.8%, 94.4% ± 2.2%, and 92.7 ± 2.5%, respectively; freedom from reoperation at the same follow-up times was 99.1% ± 1%, 97% ± 2%, and 97% ± 2% (Figure 1).
At end follow-up, there were no recorded incidences of endocarditis or stroke, and more than 97% of the patients were not receiving anticoagulant therapy and were in a normal functional class.
Authors from centers experienced in aortic valve reimplantation have reported very low in-hospital mortality after valve-sparing aortic root repair (< 2%).3,4 In our series, there was no in-hospital mortality, and 10-year mortality was 2.9%. This is significantly lower than the rate reported for aortic root replacement with a valved conduit.5
A central goal of all aortic valve conservation techniques is long-term stability. In the longest follow-up study to date, David et al.3 analyzed data from 333 patients (37.2% with MS), reporting 20-year rates for freedom from significant AoR and reoperation of 96.2% ± 1.0% and 96.9% ± 1.3%, respectively. In another center with extensive experience in this surgical procedure, 10-year freedom from reoperation was > 90%.4 In our series, the 10-year rates of significant AoR and reoperation were 7.3% and 3.8%, respectively.
Nevertheless, achieving correct coaptation sometimes requires direct repair of the aortic valve. In our series, 30.6% of the patients required procedures to repair the valve leaflets during aortic valve reimplantation. Detailed analysis of preoperative and intraoperative echocardiograms is thus essential to determine the cause of the AoR and to ensure correct initial repair and long-term stability.
In line with our results, several authors have identified valve prolapse and particularly a postoperative leaflet coaptation height < 8mm as independent predictors of long-term significant AoR and reoperation.6 There is thus an evident need to confirm optimal aortic root geometry and proper leaflet configuration after aortic valve reimplantation in order to reduce the risk of valve prolapse and subsequent mid-term and long-term AoR.
Valve-sparing aortic root repair by the David procedure provides excellent long-term clinical and functional results and should therefore be the gold standard treatment for aortic root aneurysm in MS.