We present the case of a 64-year-old man diagnosed with arrhythmogenic right ventricular cardiomyopathy in 2007, following multiple sustained monomorphic ventricular tachycardia (VT) episodes. In 2008, an endocardial ablation was performed and an automatic cardioverter-defibrillator (ICD) was implanted. After some late recurrences, a second endocardial ablation was attempted in 2015. The patient's clinical course was favorable under sotalol and subsequently amiodarone, with several recurrences, treated mainly with antitachycardia pacing until 2018, when he had incessant episodes (Figure 1A) requiring high doses of intravenous amiodarone.
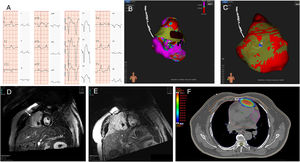
A: 12-lead electrocardiogram (25 mm/seg; 10 mm/mV) showing the clinical ventricular tachycardia and the best pacemapping during the radiofrequency ablation. B: endocardial 3D-electroanatomic voltage mapping performed with the Rhythmia System: anteroposterior view, showing previous ablation (black points represent radiofrequency applications) and, superimposed, the epicardial radiotherapy ablation (dark brown). C: epicardial layer reconstruction using the GALGO (Galgo Medical Pte Ltd) system with the same view, showing the location of the automatic cardioverter-defibrillator lead; colors define different types of tissue as follows: yellow for normal tissue, red for heterogeneous scar, and blue for dense scar. D, E: magnetic resonance before the stereotactic radiotherapy procedure and 2 months later, demonstrating a transmural scar in the right ventricular free wall (arrows). F: application of stereotactic radiotherapy volume with isodose scale.
The patient was proposed for a third endocardial ablation procedure with the Rhythmia System (Boston Scientific, Marlborough, Massachusetts, United States). The sustained monomorphic VT was not inducible and therefore we used a substrate approach. The endocardium voltage map was fairly well preserved except for the outflow tract, but the pacemapping was acceptable in the anterior midbasal free wall, quite close to the anchorage of the ICD lead (Figure 1B, C), and radiofrequency energy was delivered at this point. Two weeks after the ablation, the patient had new episodes of incessant sustained monomorphic VT, with the same morphology. Magnetic resonance imaging showed a hypocontractile right ventricle, with late gadolinium enhancement displaying a heterogeneous transmural scar in the midbasal region of the right ventricular free wall (Figure 1D).
In view of the need to perform a fourth procedure in a patient with transmural and epicardial substrate in a center without backup cardiac surgery, the decision was made to propose a noninvasive ablation with stereotaxic radiotherapy (SBRT). Various options were extensively discussed with the patient, who provided informed consent. Because a noninvasive electroanatomic mapping system was not available in our center, we defined the target region for SBRT ablation from previous endocardial ablation procedures, facing it to the right ventricle scar by magnetic resonance imaging and computed tomography (CT) scan. This information was then transferred onto 4 dimensions to define the target volume.
The patient was immobilized with a vacuum-assisted device and SBRT radioablation was performed by a LINAC (Varian Medical Systems Inc, TRUE BEAM STX), with a cone-beam CT scan to align the radiation treatment with the target volume. A single dose of 25Gy (Figure 1F) was prescribed for treatment volume, with the goal of maximal coverage within the volume while avoiding exposure to the surrounding organs at risk. The lung, esophagus, spinal cord, skin, chest wall, heart, right and left coronary arteries, and left and right ventricles were contoured as organs at risk. The treatment was performed by 2 dynamic arcs without intensity-modulated radiation therapy and 6 static fields with 10 Mv flattening filter-free photons in a Truebeam STX. An external surrogate (Varian Medical Systems Inc, RGSC) for amplitude-based gating was used during treatment to determine the breathing cycle. During radiotherapy ablation, the ICD was disconnected. Treatment lasted 4minutes and no arrhythmias were recorded during the noninvasive ablation.
The treatment was well tolerated without new episodes of VT during continuous electrocardiogram monitoring for 72h. No modifications to sense or stimulate ICD lead parameters were observed postablation (indeed, for safety reasons, the tip of the lead was excluded from the target area). Device interrogation 4 months after the irradiation showed a total absence of ventricular arrhythmias, and the magnetic resonance imaging performed during the follow-up displayed a dense transmural scar corresponding to the irradiated zone (Figure 1E). The right ventricular ejection fraction before and after treatment did not significantly change (30% and 33% before and after ablation, respectively), reflecting the low volume irradiated, which was about 3.5 cc. Because the ablation was performed exclusively in the right ventricular free wall, no changes were observed in left ventricle systolic function either.
Noninvasive ablation by SBRT may be an option to treat recurrent ventricular arrhythmias with an intramural or epicardial origin in centers without the possibility of rescue cardiac surgery or in cases of a failed epicardial approach. This treatment was first reported by Cuculich et al.1 in a small series of 5 patients with refractory VT, with either ischemic or nonischemic cardiomyopathy. After radiation, ventricular arrhythmia events dramatically decreased during follow-up, without affecting the left ventricular ejection fraction, and with a single complication consisting of mild surrounding pneumonitis, which was resolved 1 year after the procedure.
Our case differs from previously reported cases in that the main scar was localized in the free wall of the right ventricle, which is much thinner than that of the left ventricle. Nevertheless, additional recent work by Robinson et al.2 from the same group also included a patient with arrhythmogenic right ventricular cardiomyopathy, showing similar good efficacy and safety results at 90 days.
To our knowledge, this is the first noninvasive ablation procedure with SBRT performed outside the United States. It is also probably only the second procedure in the world performed in a patient with arrhythmogenic right ventricular cardiomyopathy. SBRT offers the possibility to completely homogenize the scar, without the need for the surgical precision of radiofrequency due to its transmurality, targeting not only the exit site but probably also the VT isthmus. In the last Spanish Ablation Registry 2018,3 up to 249 ablations were performed in patients with VT with a scar not related to coronary heart disease; 34 of them had arrhythmogenic cardiomyopathy. The endocardial approach was mainly used, with a high success rate. In the near future, SBRT could be an option in selected patients.
We would like to express our gratitude to Flavio Zuccarino (radiology department) and Enric Fernández-Vellila (radio-oncology physicist) for their dedication and substantial collaboration in this case (due to the journal's author policy, it was impossible to include them as coauthors).