Lipoprotein (a) (Lp[a]) has a similar composition to that of low-density lipoprotein. It contains a specific glycoprotein, apolipoprotein(a) (apo[a]), which is linked to apolipoprotein B-100 by a disulfide bridge.
Lp(a) is highly heterogeneous due to different levels of glycosylation and is polymorphic due to the presence of triple-loop structures known as kringles. There are 10 types of kringles, each with different amino acid sequences, but it is the number of kringle IV type 2 repeats that determines isoform size and potential ischemic damage.1 Lp(a) concentrations are inversely correlated with isoform size, with elevated concentrations generally correlating with small isoforms and low concentrations correlating with large isoforms. Most patients have 2 sizes of isoform.2
Lp(a) elevation may be the most prevalent monogenic lipid disorder, with estimates showing concentrations exceeding 50mg/dL in approximately 1.4 billion people worldwide.3 According to the SAFEHEART Registry, approximately 30% of patients with familial hypercholesterolemia in Spain have Lp(a) >50mg/dL.4 The pathogenic potential of this lipoprotein mainly lies in its prothrombotic, proinflammatory, and proatherogenic properties, which are linked to its structural homology to plasminogen.
The aim of this study was to estimate the prevalence of LP(a) elevation in southern Spain and examine the number and type of tests performed by hospitals in this area and the protocols used. We conducted a retrospective, observational, multicenter study of 20 hospitals in Andalusia and 3 in Extremadura. The study was approved by the ethics committee at Hospital Universitario Virgen Macarena in Seville. In June 2021, a member of staff responsible for LP(a) testing at each hospital completed a survey designed to collect data for 2019 and 2020 on laboratory data and Lp(a) testing methods and availability.
The hospitals surveyed performed 20 930 Lp(a) tests during the study period. Immunoturbidimetry was the most common method used (by 75% of hospitals), followed by nephelometry (25%), and enzyme-linked immunosorbent assay (5%).
Lp(a) testing was available at 100% of hospital laboratories compared with just 60% of primary health care laboratories; 55% of laboratories outsourced the test to another center.
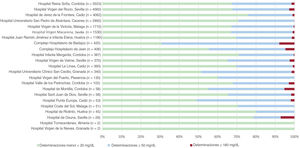
Overall, 29.58% of the tests showed an Lp(a) concentration >50mg/dL, while 1.52% showed a concentration >180mg/dL.
Hospital Reina Sofía in Cordoba performed the most tests, followed by Hospital Virgen del Rocio in Seville. Both hospitals, however, reported a similar percentage of patients with Lp(a) >50mg/dL. Lp(a) testing was underused used in certain province-level referral hospitals compared with other hospitals in the region.
The distribution of test results by hospital is shown in figure 1.
Our findings show that Lp(a) tests are underused in the hospitals analyzed. Just 9042 tests were performed in 2019 compared with 11 933 in 2020. This underuse cannot be explained by either the cost of testing (approximately €5 for once-in-a-lifetime testing) or the difficulty of including this test in the laboratories’ services portfolio.
Lp(a) measurement remains challenging, as structurally, the lipoprotein is highly heterogeneous due to its variable molecular mass (determined by apo[a] size) and lipid content. Immunoassays that use polyclonal antibodies against the hypervariable region (kringle IV) of apo(a) underestimate or overestimate Lp(a) values depending on the size of apo(a). In addition, variability in signals (isoforms with more repeats give stronger signals) introduces measurement bias, which can be minimized by applying the WHO/IFCC SRM-2B 5-point calibrator.5
The International Federation of Clinical Chemistry and Laboratory Medicine proposed that ELISA using a specific monoclonal antibody against the single epitope present on kringle IV type 9 (mAb40) should be the reference method for measuring Lp(a), as it uses antibodies that recognize just a single copy of apo(a) per particle of Lp(a).5
Lp(a) results have traditionally been reported as mass units (mg/dL) describing total lipoprotein mass, which corresponds to apo(a), apolipoprotein B-100, cholesterol, phospholipids, cholesterol esters, and triglycerides. This is metrologically incorrect, because antibody-based immunoassays measure the protein component of Lp(a), not lipid or carbohydrate content. Nanomoles per liter (nmol/L) are the most suitable unit of measurement for Lp(a) and should not be converted to mg/dL or vice versa, as all the conversion factors are inherently isoform-dependent.
Geographic studies analyzing familial clustering of Lp(a) elevation could shed light on variations in the prevalence of Lp(a) concentrations >180mg/dL.
This working group believes that scientific societies should join forces to create a protocol standardizing Lp(a) testing criteria, ordering practices, and availability in laboratory services portfolios.
In conclusion, Lp(a) tests are underused in hospitals in southern Spain. We detected a significant prevalence of Lp(a) elevation and a lack of standardization in ordering practices and testing methods.
FundingNone
Authors’ ContributionsT. Arrobas Velilla: writing of manuscript and liaison with participating hospitals to collect data. J. Fabiani de la Iglesia: creation of database for statistical analysis. S. Martín Pérez: creation of figures and interpretation of results. L. Calbo Caballos and J.J. Gómez Barrado: writing and editing of manuscript. A. León Justel: review of manuscript.
Conflicts of InterestNo conflicts of interest to declare.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2022.05.001