To the Editor,
Pulmonary hypertension rarely develops in patients with transposition of the great arteries (TGA) who undergo surgical correction with no residual defect.
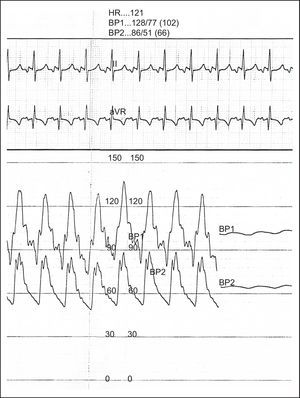
We report the case of a male patient diagnosed with TGA associated with an intact ventricular septum at birth. On the first day of life, he underwent cardiac catheterization for Rashkind balloon atrial septostomy. Pulmonary artery pressure was above systemic pressures. When the patient was 11 days old, he underwent definitive correction by means of an arterial switch procedure and closure of the atrial septal defect. He was followed-up in the pediatric cardiology department, and remained asymptomatic with no clinical signs or results in the complementary tests (including echocardiography) that might have led to suspicion of pulmonary hypertension. When aged 9 years, he started to feel tired after increasingly less effort (New York Heart Association functional class III). In the 6-min walk test, he covered 480 m and his heart rate increased from 90 to 120 bpm. In the tests performed, the electrocardiogram showed right-sided predominance. Echocardiography showed good ventricular contractility, and a ventricular eccentricity index of 1 (Figure 1). No other abnormalities were suggestive of pulmonary hypertension. In view of the discrepancy between the clinical symptoms and the complementary tests, we decided to perform cardiac catheterization, which showed pulmonary arterial hypertension above the systemic blood pressure (Figure 2) with high pulmonary artery resistance (11.7 UW), normal pulmonary capillary wedge pressure, and limited response to pulmonary vasodilators. In view of this diagnosis, we decided to initiate treatment with bosentan 62.5mg/12h and sildenafil 2mg/kg/day. After 1 year, clinical improvement was seen in the 6-min walk test, in which the patient covered 616 m with a lower increase in heart rate (65 to 81 bpm). Cardiac catheterization was repeated, and a substantial decrease in pulmonary pressures to 50% of the systemic pressures was observed, along with a decrease in pulmonary artery resistance to 5.4 UW.
Figure 1. Transthoracic echocardiography in the parasternal short-axis plane. Measurement of the eccentricity index of the left ventricle in diastole (A) and systole (B).
Figure 2. Cardiac catheterization. Simultaneous pressure trace in the descending aorta (BP2) and trunk of the pulmonary artery (BP1). HR, heart rhythm.
Pulmonary arterial hypertension associated with congenital heart disease is included in the first group of the clinical classification of pulmonary hypertension of the Dana Point Meeting, the group of pulmonary arterial hypertension. Our patient belonged to the fourth subgroup of pulmonary arterial hypertension associated with congenital heart disease, corresponding to pulmonary arterial hypertension that appears or persists after corrective surgery.1 TGA is one of the congenital heart diseases associated with late onset of hypertension; according to one series, the estimated incidence is between 3% and 4%,2 and the condition has been reported both in patients who undergo an atrial switch procedure3 and in those who undergo an arterial switch procedure.2
The pathophysiological mechanism that leads to pulmonary arterial hypertension in these patients is not fully understood; a possible etiopathogenesis are altered hemodynamics in the distribution of oxygenated blood in the fetal pulmonary vascular bed,2 while another is a more vulnerable pulmonary vascular bed during the immediate postoperative period.4
One characteristic that defines this group of pulmonary hypertension are the associated hemodynamics, which are similar to those of idiopathic pulmonary arterial hypertension. This finding is associated with worse long-term prognosis.4, 5 Indeed, pulmonary arterial hypertension has been reported as the most frequent cause of long-term mortality in patients with TGA who undergo arterial switching.6 Consequently, and given that clinical outcomes are likely to be poor, more aggressive therapeutic measures are probably needed in the treatment of pulmonary arterial hypertension with multiple therapeutic measures from the outset.
Corresponding author: macatr@msn.com