The 2012 Guidelines for Heart Failure include an indication for ivabradine according to the original design of the SHIFT study,1 and recommend that this drug be used in patients who, despite optimal treatment and maximum tolerated doses of beta-blockers, angiotensin-converting enzyme inhibitors, and aldosterone antagonists, have a heart rate (HR) in sinus rhythm above 70 bpm (Level of Evidence: Class IIa, Level B).2,3 Over the past 2 decades, a vast amount of information has accumulated on the importance of ergospirometry in the functional assessment of patients with dilated cardiomyopathy. The role of this test has begun to be recognized in the clinical context, where it is now considered an essential tool.4 The primary aim of this study was to assess functional capacity by analyzing several ergospirometry parameters and the Keteyian chronotropic index in patients with dilated cardiomyopathy and severe left ventricular systolic dysfunction treated with ivabradine compared with those treated with bisoprolol.
The study was based on a retrospective design and was conducted at a teaching hospital. All ergospirometry tests performed between July 2012 and September 2013 were reviewed, and we recruited all patients with dilated cardiomyopathy and severe left ventricular systolic dysfunction who had been receiving drug therapy for at least 6 months and were clinically stable. We excluded patients with atrial fibrillation and a cardiac resynchronization therapy device. The study was approved by the Clinical Research Ethics Committee of the hospital. The patient cohort was divided into 2 groups according to the treatment received: group I (beta-blockers) and group II (ivabradine). Patients in group II were not receiving beta-blockers due to documented pulmonary intolerance (asthma or a history of severe chronic obstructive pulmonary disease [Gold 3]). The clinical data analyzed included age, sex, smoking habits, hypertension, diabetes mellitus, hypercholesterolemia, drug therapy, body mass index, maximum oxygen uptake (VO2max) (expressed as mL/kg/min), linear regression slope of the ventilatory equivalent (VE) for carbon dioxide (VCO2), and the Keteyian chronotropic index. The formula of this index is defined as follows5: (HR at peak exercise – resting HR) / [119+(resting HR/2) – (age/2) – (5×0) – resting HR]. The statistical analysis was performed using SPSS 15.0 (Chicago, Illinois, United States).
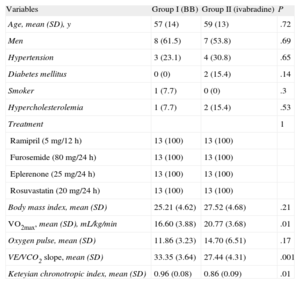
Our study population included 26 patients, 13 in each group. All study participants achieved respiratory exchange above 1.1 (which indicates adequate exertion). At the time the ergospirometry was performed, the patients had an HR below 60 bpm. The characteristics of the study population are listed in the Table. There were no statistically significant differences between the 2 groups in age, sex, cardiovascular risk factors, body mass index, or drug therapy. In terms of ergospirometry parameters, patients with dilated cardiomyopathy and severe left ventricular systolic dysfunction treated with ivabradine achieved a higher VO2max, lower VE/VCO2 slope, and a lower Keteyian chronotropic index than those treated with bisoprolol.
Baseline Characteristics of the Study Population
| Variables | Group I (BB) | Group II (ivabradine) | P |
| Age, mean (SD), y | 57 (14) | 59 (13) | .72 |
| Men | 8 (61.5) | 7 (53.8) | .69 |
| Hypertension | 3 (23.1) | 4 (30.8) | .65 |
| Diabetes mellitus | 0 (0) | 2 (15.4) | .14 |
| Smoker | 1 (7.7) | 0 (0) | .3 |
| Hypercholesterolemia | 1 (7.7) | 2 (15.4) | .53 |
| Treatment | 1 | ||
| Ramipril (5 mg/12 h) | 13 (100) | 13 (100) | |
| Furosemide (80 mg/24 h) | 13 (100) | 13 (100) | |
| Eplerenone (25 mg/24 h) | 13 (100) | 13 (100) | |
| Rosuvastatin (20 mg/24 h) | 13 (100) | 13 (100) | |
| Body mass index, mean (SD) | 25.21 (4.62) | 27.52 (4.68) | .21 |
| VO2max, mean (SD), mL/kg/min | 16.60 (3.88) | 20.77 (3.68) | .01 |
| Oxygen pulse, mean (SD) | 11.86 (3.23) | 14.70 (6.51) | .17 |
| VE/VCO2 slope, mean (SD) | 33.35 (3.64) | 27.44 (4.31) | .001 |
| Keteyian chronotropic index, mean (SD) | 0.96 (0.08) | 0.86 (0.09) | .01 |
BB, beta-blockers; VCO2, carbon dioxide output; VE, ventilatory equivalent; VO2max, maximum oxygen uptake.
Unless otherwise indicated, the data are expressed as No. (%).
Our study can be considered a proof-of-concept study, as it shows that patients with dilated cardiomyopathy and severe left ventricular systolic dysfunction after 6 months of ivabradine therapy exhibit better functional and ventilatory capacity. Our results are consistent with those of a study by Volterrani et al,6 which showed that ivabradine alone or in combination is more effective than carvedilol in improving exercise tolerance among patients with heart failure.
Our study is unique in that all patients had an HR below 60 bpm in the ergospirometry test, unlike that by Volterrani et al,6 who observed higher HR values. Likewise, we used a new equation, the Keteyian chronotropic index. This is a recently defined equation to predict maximal HR in patients with heart failure who take beta-blockers.5 Our analysis showed that exercise capacity improved among patients receiving ivabradine therapy, possibly due to a slower increase in HR during exercise, as expressed by the Keteyian chronotropic index. From the pathophysiologic point of view, this may slow the increase in left ventricular filling pressure, delaying the onset of dyspnea and the end of exercise.