We report the case an 87-year-old man with severe aortic stenosis and dyspnea, New York Heart Association functional class III, and a class I indication for valve replacement. His medical history included hypertension, chronic obstructive pulmonary disease, and bilateral knee replacement; his logistic EuroSCORE was 13.92%. The technique chosen by the medical-surgical team was transfemoral transcatheter aortic valve implantation.
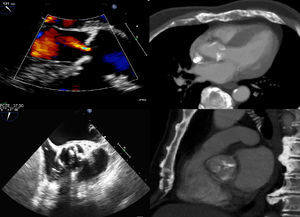
Preimplantation transthoracic echocardiography showed a critical aortic stenosis of 0.40cm2 (0.25cm2/m2 when corrected for body surface area), generalized moderate left ventricular hypertrophy, and mild systolic dysfunction. Computed tomography angiography showed a sparsely calcified right common femoral artery of good caliber and a low degree of tortuosity in the aortoiliac segment. The minimum diameters of the right common femoral, right external iliac, and right common iliac arteries were 7mm, 9mm, and 11mm, respectively. The distance from the annulus to the coronary ostia was 11.5mm from the left coronary artery and 13mm from the right coronary artery. There was asymmetric moderate valvular calcification and the left coronary and noncoronary leaflets were the most affected; the annulus was 21×23mm and there was no subannular aortic calcification (Figure 1).
Transesophageal echocardiography showed an annulus of 21 to 22mm and asymmetric severe valvular calcification mainly of the left coronary and noncoronary leaflets (Figure 1), which was similar to that found on computed tomography angiography.
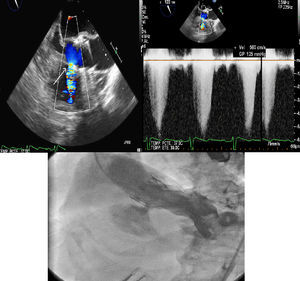
An Edwards-SAPIEN prosthesis number 26 (Lifesciences, Irvine, California, United States) was implanted via the right femoral artery using the standard procedure, with good outcome, although subsequent ventriculography showed a ventricular septal defect (VSD) in the membranous septum that had not been previously observed. Transesophageal echocardiography showed a small restrictive VSD with a 0.6cm diameter and a 125mmHg gradient. Predischarge transthoracic echocardiography showed no change in gradient (Figure 2).
Two years after implantation, the patient was asymptomatic, with functional class I, and had resumed a normal life for his age; transthoracic echocardiography follow-ups showed that the VSD remained restrictive (gradient, 110mmHg).
This complication was probably due to the selected valve being oversized (26mm for an annulus of 21 to 22mm) and, upon inflation, the struts tearing the membranous septum despite the valve not being overexpanded or implanted in a low position. The asymmetric valvular calcification and the asymmetric expansion of the prosthetic valve during the implantation procedure may also have contributed to the development of this complication. Subannular aortic calcification could also have been a factor, but this possibility was ruled out by transesophageal echocardiography and computed tomography angiography (Figure 1).
Two other cases of VSD following transfemoral transcatheter aortic valve implantation have been described,1,2 although unlike the present case, the VSD became clinically evident 1 week after the procedure in the first case and was sonographically confirmed 6 weeks after the procedure in the second case. In the first case, percutaneous closure of the VSD was performed with an Amplatzer device due to significant left-right shunt. In the second case, medical treatment and clinical and imaging follow-up was applied, although the VSD was restrictive and associated with a ruptured aortic root involving the formation of a pseudoaneurysm. The VSD was not shown in either case by transesophageal echocardiography or by the final angiography during the transcatheter aortic valve implantation procedure.
One case has been reported3 of a patient dying 2 days after transapical aortic valve implantation due to ventricular arrhythmia and heart failure. The autopsy showed a hematoma of the septum with a small VSD.
In conclusion, we wish to stress that this is an uncommon complication. In our patient, it followed a benign course over 2 years. We also want to emphasize that extreme care should be taken when measuring the aortic valve annulus and assessing the symmetry of valvular calcification, whether by transthoracic echocardiography or computed tomography angiography, in order to avoid these types of potentially severe complications (ruptured aortic root, aortic dissection, etc.).
CONFLICTS OF INTERESTDr Eulogio García Fernández is proctor in Spain for Edwards-SAPIEN prosthetic aortic valves.