To the Editor,
Myocardial bridge (MB) is the most common, and potentially benign, congenital anomaly of coronary arteries.1 We present the case of a 26-year-old woman, referred to our hospital with a history of a few years of orthostatic hypotension and recurrent syncope or presyncope usually induced by short periods of intensive physical activity or mental stress without any prodromal symptoms.
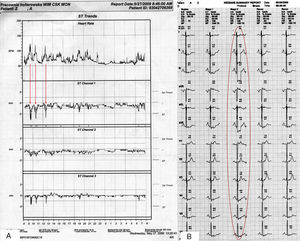
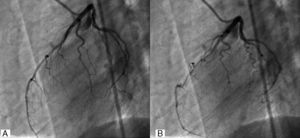
Echocardiography was performed; head-up tilt test did not reveal any pathology. During 24-h ECG Holter monitoring, significant ST depressions related to sinus tachycardia were found (Figure 1A). Recommended exercise treadmill test was interrupted by sudden syncope at 3min with coexisting ST depressions of almost 10mm in limb leads (Figure 1B). Patient underwent computed tomography, which showed long, significant MB at left anterior descending artery, confirmed in coronarography (Figure 2). Due to her young age, noninvasive treatment with a low dose of β-blocker was prescribed. Prolonged ECG telemonitoring also was performed. Unfortunately, due to poor tolerance of the treatment (exacerbation of orthostatic hypotension) and persistent presence of recurrent ECG changes during normal activity she again consulted with the cardiac surgeon, and was finally approved for by-pass grafting. In November 2009 she was operated on, and the left internal mammary artery was successfully embedded. After discharge she was controlled with ECG telemonitoring for 3 months; ischemic changes were absent. During 2 years of follow-up she was free of symptoms, and significant physical efficiency improvement was noted.
Figure 1. ST changes during (A) Holter electrocardiographic monitoring and (B) treadmill test.
Figure 2. Coronarography of the left anterior descending artery during (A) diastole and (B) systole.
In our patient MB had provoked syncope related to severe ischemia (with almost 10mm ST depression) during low-intensity physical activity. The left anterior descending artery is the most common coronary artery affected by MB,2 which often occurs without overt symptoms and is generally a benign condition.3 The clinical significance of the bridge is determined by the affected arteries’ anatomy, concomitant atheromatous changes and possible myocardial ischemia. During systole, contraction of the overlying myocardium compresses the artery, which may persist into diastole, when the majority of coronary blood flow occurs. Increased heart rate, short diastolic perfusion time, increased myocardial contractility and flow velocity, and exercise-induced coronary spasm can all cause angina in patients with MB. This hypothesis is compatible with our case observation, in which important ischemia was strictly heart rate dependent. In symptomatic patients, management of MBs is usually pharmacological.3 Available medications include negative inotropes (β-blockers and Ca-blockers). Nitrates should be avoided because they increase the degree of systolic narrowing and can worsen the symptoms. Another alternative is a surgical myectomy; however, the complication rate is higher than any other intervention and the prognostic value is limited.4 Percutaneous coronary intervention could be suggested as an alternative therapeutic option. Nevertheless, the results of balloon angioplasty are unsatisfactory, because elastic recoil limits the control of symptoms. Bare-metal stent implantation should not be considered as the treatment of choice because of restenosis rate. Drug-eluting stents could be a solution; however, some authors report the possibility of stent fracture (especially in sirolimus-eluting stents).5 Metal fatigue from repetitive mechanical stress during systole has been suggested as a possible mechanism of stent failure. It has also been suggested that long stents, segments with marked angulations, and overlap zones are risk factors for stent fracture.5 As mentioned above, in our patient preservative treatment was unsuccessful and finally coronary artery bypass graft was used. Significant postoperative improvement confirmed the etiology of the presented symptoms. Some authors6 have presented cases of significant ischemia in middle-aged patients; our patient was severely ischemic during normal activity in her twenties without any other risk factor of coronary artery disease, so even this radical therapeutic decision had to be performed as quickly as possible. We believe that in symptomatic cases resistant to pharmacotherapy, an invasive procedure should be performed independently of the age of the patient.
.
Corresponding author: astanczyk@wim.mil.pl