Catecholamine-producing tumors have a low incidence and rarely involve myocardial toxicity. The inverted variant of tako-tsubo syndrome is uncommon and occurs in younger patients. ST-T depression is the most typical abnormality seen on electrocardiography. This variant is also associated with an increased incidence of cardiogenic shock, arrhythmias, and kidney failure.1
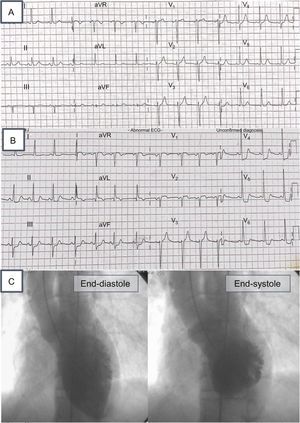
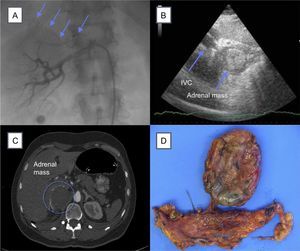
We describe the case of a 52-year-old woman with a history of chronic hypertension currently under treatment with enalapril. A recent echocardiogram showed no structural heart disease. She was admitted to the emergency service for sudden-onset severe headache and general malaise. At admission, blood pressure, electrocardiogram (Figure 1A), and chest X-ray were normal. During her stay in the emergency room, she developed disorientation, clouding of consciousness, and vomiting. Documented blood pressure was 210/100mmHg. Blood test values were within normal limits and the results of cranial CT scan were unremarkable. Subsequently, the patient had a chest pain episode with ischemic features. Electrocardiogram was repeated and showed ST depression in V5-V6, II, III, and aVF (Figure 1B). An emergency echocardiogram showed moderate-severe ventricular dysfunction with preserved apical contractility (Video 1 of the supplementary material). Based on these findings, cardiac catheterization was performed with no evidence of obstructive lesions or vasospasm and with good coronary flow (TIMI III; Video 2 and Video 3 of the supplementary material). Ventriculography showed findings similar to those of the electrocardiogram and were compatible with inverted tako-tsubo syndrome (Figure 1C). Given the hypertensive crises, renal artery angiography was performed with no evidence of stenosis, but showed a vascular neoformation extending to the right upper renal pole (Figure 2A). Peak creatine kinase was 613 U/L and peak ultrasensitive troponin was 1707 ng/dL. Several hours after cardiac catheterization, the patient had another hypertensive crisis and hemodynamic deterioration requiring invasive mechanical ventilation, vasoactive support with noradrenaline at 1.1μg/kg/min, dobutamine at 18μg/kg/min, and intraaortic balloon counterpulsation (IABC). A new echocardiogram performed in the subcostal plane showed a mass of about 5cm adjacent to the inferior vena cava (Figure 2B). An abdominal CT scan showed a right adrenal mass (Figure 2C). The patient remained hemodynamically unstable (cardiogenic shock and 2 episodes of ventricular tachycardia and cardiorespiratoy arrest), for which venoarterial extracorporeal membrane oxygenation (ECMO) was commenced with distal cannulation 24hours after IABC. There was a stepped decrease in catecholamine levels. On the third day of circulatory support with ECMO, ventricular function recovered (Video 4 of the supplementary material), and so circulatory and vasoactive support were progressively withdrawn. Right adrenalectomy was performed after the patient was started on therapy with alpha-blockers and subsequently with beta-blockers. The pathologic findings (poorly differentiated necrotic cells) and the results of blood analysis (chromogranin A, 594 ng/mL [0-100]; metanephrine, 203 pg/mL [0-90], and normetanephrine, 414 pg/mL [0-180] in plasma) were compatible with pheochromocytoma.
A: right renal arteriography. Arrows show abnormal adrenal vascularization; B: cardiogram in subcostal plane showing IVC and adrenal mass; C: abdominal CT. The circle shows the location of the adrenal mass; D, macroscopic specimen of the tumor. CT, computed tomography; IVC, inferior vena cava.
We present a case of inverted tako-tsubo syndrome with cardiogenic shock, likely caused by a massive release of catecholamines due to pheochromocytoma. This phenomenon in association with pheochromocytoma was first described by a Spanish group in 2006.2 The use of exogenous catecholamines during diagnostic tests could lead to false positives, and thus endogenous catecholamine levels should be determined after the withdrawal of vasoactive support and then compared after the tumor has been removed. In the present case, normal values were restored during follow-up. Various mechanisms of catecholamine-mediated toxicity have been proposed, such as excessive sympathetic stimulation, and increased inotropism, chronotropism, and afterload.3 Alpha-adrenergic activation could cause vasospasm and direct myocardial toxicity via an increase in the permeability of the sarcolemmal membrane and in intracellular cardiac calcium concentrations.4 Apical and midventricular susceptibility in catecholamine-induced myocardial toxicity has been associated with differences in the distribution of the sympathetic system and beta-adrenergic receptors. The inverted variant could be explained by such variations in distribution.5 In this setting, the use of ECMO, with or without balloon counterpulsation, has proven effective until the recovery of ventricular function, allowing alpha- and beta-blockade before tumor resection.6 There is no consensus on the timing of surgery in patients with heart failure and the choice of urgent surgery remains controversial. Histological findings suggested that the necrosis of the surgical specimen could be related to the massive catecholamine release.4 Consequently, the subsequent relative adrenergic failure could contribute to persistent shock.