Acute myocarditis is an inflammatory disease of the myocardium with a variable presentation and clinical course. Although the symptoms spontaneously resolve in between 50% and 60% of patients, 20% to 40% die or require heart transplantation.1,2 Most patients with a favorable course improve during the first 2 to 4 weeks. A worse clinical course has been associated with the presence of ventricular dysfunction.1–3
From July 2008 to March 2016, 32 infants and children (0-16 years) with acute myocarditis were admitted to our center. Of these, 53% (17 of 32) had a left ventricular ejection fraction (LVEF) < 35%; 47% of these patients (8 of 17) died or required transplantation. Although acute myocarditis is definitively diagnosed with endomyocardial biopsy (EMB), the technique is not performed systematically because of some associated risks.3 Some immunosuppressive or antiviral therapies can be useful in the subacute or chronic phase.4–6
Interferon-1β (IFN-1β) is a molecule secreted by immune system cells, mainly fibroblasts. Its serum levels are decreased in patients with myocarditis and persistent virus in the myocardium6 and it is therapeutically useful in patients with dilated cardiomyopathy and polymerase chain reaction (PCR) detection of a viral genome.5,6 In addition, immunosuppressive therapy can be useful in patients with inflammatory cardiomyopathy and negative viral PCR results.4 Accordingly, from February 2015, a specific protocol-directed therapy was implemented in those patients in our center with acute myocarditis and LVEF < 35% with no echocardiographic evidence of improvement after 2 weeks. The suspected diagnosis was made according to clinical symptoms and suitable complementary examinations, including cardiac magnetic resonance imaging.3 Before the therapeutic approach was chosen, EMB was performed in patients with an unfavorable clinical course. We performed histological and immunohistochemical studies and viral PCR analysis. Myocarditis was diagnosed by the presence of > 14 leukocytes with > 7 lymphocytes/mm2.
Patients with inflammation and negative PCR were treated with methylprednisolone and mycophenolate mofetil for 6 months. Because mycophenolate has fewer adverse effects,4 it was used instead of azathioprine. If a positive viral PCR result was obtained in the myocardium, treatment was begun with subcutaneous IFN-1β for 6 months (Betaferon at a dosage of 4 million units 3 days a week5,6) and specific antiviral treatment if available. Methylprednisolone was added if there was inflammatory infiltrate.
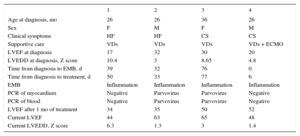
Here, we detail our experience with 4 patients. Their characteristics are shown in the Table. Three were transferred from other centers for transplant evaluation and the fourth was admitted with cardiogenic shock. All had severe involvement of the left ventricle with a mean LVEF at admission of 24.7% (SD: ± 7.3) and a mean left ventricular end-diastolic diameter Z score of 6.7 (SD: ± 3.4). The patient with cardiogenic shock required circulatory assistance with extracorporeal membrane oxygenation. In this patient, EMB was performed on the first day together with balloon atrial septostomy. In the remaining patients, EMB was performed 53 days (SD: ± 22) after diagnosis. The access was femoral in the patient with extracorporeal membrane oxygenation and jugular in the rest. The samples were obtained from the right side of the interventricular septum. There were no intraprocedural complications. Two patients had inflammation with negative PCR findings in the myocardium and peripheral blood; the other 2 had inflammation with positive PCR for the B19 parvovirus in the myocardium and peripheral blood. Specific therapy was begun after the EMB result. The mean LVEF before treatment was 26% (SD: ± 6). Currently, 3 patients have completed the therapy and the fourth has received it for 4 months. After a mean follow-up of 7 months (SD: ± 2.4), the mean ejection fraction was 55.2% (± 10.2%, P = .01). Two patients are now cured and 2 have improved, with some residual dysfunction. The 2 cured patients were infected with B19 parvovirus and were treated with IFN-1β. Regarding complications, the patients treated with IFN-1β showed increased transaminase levels (maximum AST/ALT values of 500/150 UI/L); the levels normalized after temporary withdrawal of the drug (5 days) and remained stable upon reintroduction of IFN-1β.
Baseline and Post Treatment Characteristics of the Patients
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| Age at diagnosis, mo | 26 | 26 | 36 | 26 |
| Sex | F | M | F | M |
| Clinical symptoms | HF | HF | CS | CS |
| Supportive care | VDs | VDs | VDs | VDs + ECMO |
| LVEF at diagnosis | 17 | 32 | 30 | 20 |
| LVEDD at diagnosis, Z score | 10.4 | 3 | 8.65 | 4.8 |
| Time from diagnosis to EMB, d | 39 | 32 | 76 | 0 |
| Time from diagnosis to treatment, d | 50 | 33 | 77 | 6 |
| EMB | Inflammation | Inflammation | Inflammation | Inflammation |
| PCR of myocardium | Negative | Parvovirus | Parvovirus | Negative |
| PCR of blood | Negative | Parvovirus | Parvovirus | Negative |
| LVEF after 1 mo of treatment | 34 | 35 | 50 | 52 |
| Current LVEF | 44 | 63 | 65 | 48 |
| Current LVEDD, Z score | 6.3 | 1.3 | 3 | 1.4 |
CS, cardiogenic shock; ECMO, extracorporeal membrane oxygenation; EMB, endomyocardial biopsy; F, female; HF, heart failure; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; M, male; PCR, polymerase chain reaction; VDs, vasoactive drugs.
In conclusion, we consider that IFN-1β and immunosuppressive therapy can have beneficial results in patients with acute myocarditis. Endomyocardial biopsy is essential before treatment initiation. Prospective randomized multicenter studies are required to determine the usefulness of these treatments in pediatric patients.