To the Editor,
The concept of inappropriate left ventricular mass (iLVM)1 was introduced to distinguish between compensatory increases in LVM and clinically relevant, maladaptive changes.2 iLVM is that which exceeds the expected value for a given individual based on sex, body size, and stroke work, and it is associated with an increased cardiovascular risk.3, 4
We determined the prevalence of iLVM and assessed its relationship with left ventricular function (LVF) in 411 students (265 women; mean [SD] age, 20.62 [0.07] years) from the Facultad de Ciencias Médicas at the Universidad Nacional de La Plata in Argentina. A sample size of 174 individuals was calculated as sufficient to detect a prevalence of 6% with a 95% confidence level and a precision of 3%; group sizes of 25 to 50 were calculated as sufficient to detect minimal differences in parameters associated with LVF with an α risk of 0.05 and a β risk of 0.20. We analyzed family history of cardiovascular risk factors (RF), weight, height, waist and hip circumference, and blood pressure in all participants. Doppler flow and tissue Doppler echocardiography were used to characterize left ventricular structure and LVF. LVM was calculated according to Devereux et al.5 and the LVM index (LVMI) was calculated by dividing the LVM by the individual's height in meters to the power 2.7; LVMI >47g/m2,7 in women and >50g/m2,7 in men is indicative of left ventricular hypertrophy. iLVM was calculated according to De Simone2; our cutoff was set at the 95th percentile (117%) according to the mass expected for the population with weight and blood pressure in the normal range. Systolic function was assessed by determination of the mean velocity of fiber shortening corrected for stress at peak systole (Vcf) and the peak systolic mitral annular velocity (S’); diastolic function was determined from the ratio of peak early mitral inflow velocity (E) and peak early mitral annular velocity (e’) (E/e’). Continuous variables were expressed as means (SD) and categorical variables as percentages. Differences between continuous variables were analyzed by t test and the χ2 test was used to compare categorical variables. Analysis of covariance was used to adjust the values of iLVM for body surface area, ratio of waist to hip circumference, and systolic blood pressure, and univariate analysis was used to assess the correlation between stroke work ratio and LVM. Data were analyzed using SPSS version 15.0. In all cases a cutoff of P<.05 was used to determine statistical significance.
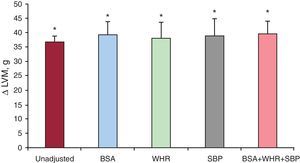
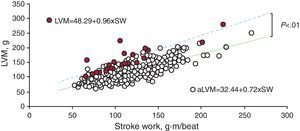
The prevalence of iLVM in our students was 6% (95% confidence interval, 3.7%-8.2%). There were no significant differences in age, weight, height, sex, blood pressure, or family history of cardiovascular RF in those with appropriate (aLVM) and iLVM. Adjustment for covariables in students with iLVM (Figure 1) did not alter the excess LVM of 36.7 (2.15) g observed in that group. The LVM at a given stroke work was greater in students with iLVM (Figure 2; P<.01). The LVMI (29.09 [0.30] g/m2,7 in students with aLVM; 40.39 [1.91] g/m2,7 in students with iLVM; P<.01), prevalence of LVH (0.5% in students with aLVM; 8% in students with iLVM; P<.01), wall thickness (8.50 [0.05] mm in students with aLVM; 10.13 [0.23] mm in students with iLVM; P<.01), and relative wall thickness (0.37 [0.002] in students with aLVM; 0.44 [0.01] in students with iLVM; P<.01) were all greater in students with iLVM. There was also a reduction in S’ (24.69 [0.41] cm/s in students with aLVM; 21.15 [1.65] cm/s in students with iLVM; P<.03) and Vcf (101.59% [0.9%] in students with aLVM; 91.94% [4.71%] in students with iLVM; P<.01), as well as an increase in E/e’ (2.76 [0.05] in students with aLVM; 3.27 [0.30] in students with iLVM; P<.01) compared with students who had an aLVM.
Figure 1. Differences in left ventricular mass in young adults with appropriate and inappropriate left ventricular mass with and without adjustment. BSA, body surface area; LVM, left ventricular mass; SBP, systolic blood pressure; WHR, waist-to-hip ratio. *P<.05.
Figure 2. Relationship between stroke work (horizontal axis) and left ventricular mass. Filled circles correspond to young adults with inappropriate left ventricular mass. aLVM, appropriate left ventricular mass; LVM, left ventricular mass; SW, stroke work.
The main findings of this study indicate that 6% of students with no apparent cardiovascular disease had iLVM with shortening of the circumferential and longitudinal fibers as an expression of the deterioration in systolic function, and an increase in left ventricular diastolic pressure as an expression of diastolic dysfunction. These findings were independent of family history of cardiovascular RF, blood pressure, or anthropometric variables. The persistence of increased LVM in the group with iLVM when adjustments were made for different covariables indicates an inadequate response. The reduction in S’ and Vcf in young people with iLVM is an important indication of a general abnormality of the myocardial fibers and is associated with lower afterload following similar preload when compared with the group with aLVM. This finding is indicative of inotropism. Although the absolute values of E/e’ in our study are within the normal range, the increase observed in individuals with iLVM would suggest a slight increase in ventricular filling pressure as an expression of early changes in diastolic function. Although the cross-sectional nature of the study makes it impossible to determine the risk of cardiovascular events in the population studied, the emerging phenotype of the individuals with iLVM is similar to that previously shown in adults, where it was associated with increased risk.3, 4 These findings support the concept of an inadequate response in the development of iLVM, described here for the first time in young adults. Longitudinal studies are now required to assess the prognostic impact of this subclinical marker of compromised cardiac function in similar populations.
Corresponding author: emescu@gmail.com