Increased low-density lipoprotein cholesterol (LDLc) is associated with symptoms and death due to cardiovascular disease (CVD).1 Reduction of LDLc with statins decreases the risk of cardiovascular events.2 The guidelines for the management of dyslipidemia of the European Society of Cardiology, which were in force at the start of the COLIPAR project presented here, recommend LDLc < 70mg/dL for very high-risk patients.1
This goal is, however, attained in only a low percentage of patients: 33% in the DYSIS registry3 and 26% in the REPAR registry.4 Furthermore, a very high percentage of patients diagnosed with CVD maintain levels above 70mg/dL, although clinicians are often unaware that this poor control can negatively affect their patients.
In view of the above, we decided to assess the degree of lipid control in our very high-risk patients and to share the findings with our colleagues in primary and specialist care to determine whether awareness of the degree of lipid control might help to achieve lipid targets.
All patients with documented CVD in our health area were identified with the clinical management system (Outpatient Information System-Abucasis), which covers all diagnoses. For the present study, a patient was considered at high risk if at least 1 of the following conditions was diagnosed: ischemic heart disease, cerebrovascular disease, or peripheral artery disease. All LDLc measurements were retrieved over a 1-year period (September 2012 to September 2013). The percentage of patients with satisfactory control (cLDL < 70mg/dL) was estimated. A total of 8 face-to-face meetings and 3 online seminars were held during a 1-year period (March 2014 to April 2015). During these seminars, our colleagues in primary and specialist care were informed of the percentage of patients with satisfactory control in their health center or service, and of the benefits of improving lipid control. After 1 year, data were extracted again from the system to assess whether there was any improvement (Figure 1).
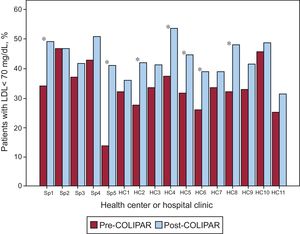
Of a total of 311 672 individuals in our health area, we identified 4258 patients with CVD. Of these, only 1820 (43%) had at least 1 laboratory determination that included LDLc during baseline data extraction (September 2012 to September 2013). Initially and in general, 33.6% had adequate LDLc control (mean, 86.7±30.3mg/dL). One year after the seminars revealing the degree of control to all health centers and specialties and emphasizing the importance of improving control, 1595 of the 1820 patients (88%) had undergone measurement. In these patients, the degree of lipid control improved significantly, to 45.6% of patients with satisfactory control (P<.0001). Mean LDLc was 77.9±28.5mg/dL. As seen in Figure 2, which presents data by individual center, many specialties and health centers improved the percentage of patients with well-controlled LDLc.
In line with all published registries, the present study highlights inadequate lipid control in patients with high cardiovascular risk in our cohort. The novelty of this study, however, is that it demonstrates how a joint effort between specialists and primary care, who were made aware of the percentage of well-controlled patients and the importance of good lipid control, resulted in treatment optimization in these patients and a significant improvement in lipid levels. The most important shortfall detected was the absence of lipid measurements, affecting 57% of patients at baseline and 12% after the program, when clinical practice guidelines clearly recommend annual LDLc measurements in these patients.1 In contrast, the main achievement detected in this study is that the percentage of patients with LDLc< 70mg/dL increased from 34% to 46%. This improvement was most evident in centers with lower percentages of patients with good control to start with, and where the message about satisfactory lipid control had the greatest impact (Figure 2).
The baseline figures for failure to attain the lipid goals in patients with very high cardiovascular risk are very similar to those in the DYSIS registry,3 but they are far below the recommendations of the European Society of Cardiology.1
We believe that patients and physicians are both responsible for the failure to attain lipid goals. Often, once the initial stages of the disease have passed, patients may relax and not follow recommendations on diet, exercise, and even medication. For their part, physicians suffer from therapeutic inertia due to the lack of time with the patients and lack of awareness of the importance of satisfactory lipid control. These factors prevent them from intensifying treatment to achieve treatment goals. An intervention such as that described in this study, stressing the importance of good control and presenting real data from our patients, has proven useful for improving lipid control.
The main limitation of this study is the lack of information on how long ago the clinical events occurred or on the history or treatments of the patients included.
In summary, lipid control in very high-risk patients in a clinical practice cohort was unsatisfactory, but cooperation with primary care, with appropriate information and heightened awareness, seems essential to improve control.
.