Various studies have shown improved left ventricular ejection fraction (LVEF) in ischemic heart disease following infusion of autologous mononuclear bone marrow cells.1,2 There is little information on the long-term results of this approach in nonischemic dilated cardiomyopathy.3–5 Our objective was to analyze the long-term results, as well as the clinical angiographic, echocardiographic, and biological factors associated with good outcomes.
The present study involved a mean follow-up of 53±14 months in 27 patients with dilated cardiomyopathy in optimal clinical treatment and with symptomatic heart failure who underwent intracoronary infusion of autologous mononuclear bone marrow cells between 2008 and 2010. All patients were participants in the TCMR0007/06 trial. Baseline characteristics have been described in a publication from our group.6
The baseline clinical, echocardiographic, hemodynamic (Table), and biological data6 were analyzed to evaluate their influence on late response.
Baseline Clinical and Echocardiographic Parameters
| Group I (n=15) | Group II (n=12) | P | |
|---|---|---|---|
| Age, mean±SD, y | 49±12 | 58±11 | <.05 |
| Men, % | 73 | 75 | NS |
| NYHA | 2.2±0.4 | 2.7±0.7 | <.05 |
| BNP, pg/mL | 341±415 | 481±424 | NS |
| Cholesterol, mg% | 167±47 | 183±28 | NS |
| LDL-C, mg% | 99±30 | 115±19 | NS |
| HDL-C, mg% | 37±10 | 36±13 | NS |
| Triglycerides, mg% | 145±107 | 168±108 | NS |
| Hypertension, % | 53 | 58 | NS |
| Hyperlipidemia, % | 60 | 75 | NS |
| Smoking, % | 73 | 58 | NS |
| Diabetes mellitus, % | 27 | 50 | NS |
| LVEF, % | 30±5 | 23±9 | <.05 |
| LV end-diastolic volume, mL | 164±78 | 214±64 | NS |
| LV end-systolic volume, mL | 112±52 | 165±56 | <.05 |
| Degree of mitral regurgitation | 0.53±0.7 | 0.50±0.5 | NS |
| LVEF in sinus rhythm, % | 31±9 | 24±7 | <.05 |
| LVEF in sinus rhythm post-PVC, % | 46±13 | 35±11 | <.05 |
| Sinus end-diastolic volume, mL/m2 | 143±49 | 183±76 | <.05 |
| Post-PVC end-diastolic volume, mL/m2 | 163±48 | 194±74 | NS |
| End-systolic sinus volume, mL/m2 | 99±41 | 142±64 | NS |
| Post-PVC end-systolic volume, mL/m2 | 90±40 | 127±60 | NS |
| Systolic pressure of the pulmonary artery, mmHg | 34±18 | 37±13 | NS |
BNP, brain natriuretic peptide; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; LV, left ventricle; LVEF, LV ejection fraction; NS, no significant; NYHA, New York Heart Association functional class; post-PVC, post-premature ventricular contraction.
All echocardiographic parameters were determined using the Simpson method.
Group I: patients without follow-up events. Group II: patients with follow-up events.
Data are expressed as mean±standard deviation and as percentages; P<.05 was considered statistically significant.
Fifteen patients (56%) showed no major events (group I) and 12 (44%) did (group II). Patients were considered responders if their LVEF had improved more than 5% at the 6-month angiographic evaluation; 21 patients were responders (14 from group I) and 6 were nonresponders (5 from group II).6 The events in group II were as follows: 3 deaths (due to heart failure), 2 at 21 months and 1 at 69 months (a cardiac resynchronization device was implanted in this patient at 18 months after the infusion); 3 patients were admitted at least once due to heart failure (29±11 months); and 6 patients required cardiac resynchronization therapy (25±7 months). After various admissions for heart failure, 1 of the patients with a cardiac resynchronization device received a heart transplant (41 months). All group I patients were in functional class I-II, whereas most of those in group II were in functional class II-III (1.6±0.6 in group I vs 2.3±0.9 in group II; P<.05). The lastnatriuretic peptide value was 156±450 pg/mL (69±58 pg/mL in group I vs 280±750 pg/mL in group II; P<.05). The mean of the last LVEF by transthoracic echocardiography was 35%±13% (42%±11% in group I vs 26%±5% in group II; P<.05), with a global LVEF gain (follow-up LVEF minus baseline LVEF) of 7.4%±11% (11.6%±12.1% in group I vs 2.5%±7.4% in group II; P<.05). There were no differences in cell biological parameters or adverse events directly associated with the treatment.
Differences were found in age (48±11 years in group I vs 58±11 years in group II; P<.05); baseline echocardiogram, with lower mean baseline systolic volume (112±52mL in group I vs 165±56mL in group II; P<.05) and higher LVEF (30%±5% in group I vs 23%±9% in group II; P<.05) and baseline angiogram, with higher LVEF and post-premature ventricular contraction LVEF (31%±9% vs 24%±7%; P<.05; and 46%±13% vs 35%±11%; P<.05) and lower diastolic volume (143±49 mL/m2 in group I vs 183±76mL/m2 in group II; P<.05). Group I had a better baseline New York Heart Association functional class (2.1±0.4 vs 3.0±0.7; P<.05).
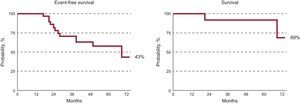
At 5 years follow-up, 43% of patients were free of major events. At 6 months, 52% of responders were event-free; at 5 years, only 17% of the nonresponders were event-free. Benefits appeared to be maintained over time, with a 69% 5-year survival rate (Figure). In previous series of nonischemic dilated cardiomyopathy patients treated with conventional therapy, the 5-year survival varied between 55% and 65%. In our series, more than half of the patients with idiopathic dilated cardiomyopathy treated with infusion of autologous mononuclear bone marrow cells showed a favorable clinical course 5 years later and were in functional class I-II and free of major events. A better late clinical course was shown by younger patients, in better clinical condition, with smaller ventricular diameters and better baseline LVEF. Infusion of these cells can be considered a promising and safe therapy because there were no adverse events related to the therapy in our series. However, the results of our study should be carefully interpreted due to the lack of a control group.
.