Identification of noninvasive prognostic markers in patients with left ventricular dysfunction (LVD) is a challenge for the clinician. Although LVD is in itself an important predictor of adverse cardiac events, other markers are needed to refine risk stratification, as a poor correlation between the degree of LVD and adverse cardiac events is often observed in clinical practice.
The presence of myocardial fibrosis in cardiac magnetic resonance imaging (MRI) with late gadolinium enhancement1,2 and the deterioration of sympathetic cardiac innervation quantified by 123I-metaiodobenzylguanidine (123I-MIBG) scintigraphy3–6 have been introduced as new risk markers in recent years. We designed a prospective observational study with the aim of assessing whether the combination of information from these 2 techniques can improve risk stratification when an implantable cardioverter defibrillator is indicated for primary prevention.
We studied 47 consecutive patients with cardiac failure in New York Heart Association functional class II or III at baseline, left ventricular ejection fraction =35%, optimum pharmacological treatment, and class I indication for implantable cardioverter defibrillators, who had undergone prior cardiac MRI and 123I-MIBG scintigraphy. Events were recorded during follow-up. The study was approved by the ethics committee of our hospital and patients provided their informed consent in writing. Here, we present the findings of cardiac innervation and its association with cardiac events during follow-up.
Scintigraphy of cardiac innervation was performed by intravenous injection of 10 mCi of 123I-MIBG and subsequent image acquisition in the anterior region of the chest at 15min and 4h after injection of the tracer. Myocardial uptake of 123I-MIBG was quantified by the early and late heart-to-mediastinum ratio (HMR) and the washout rate.
Categorical variables are expressed as percentages and quantitative ones as mean (SD). Variables were compared using the ?2 test (categorical) or the Fisher and Student t test (quantitative). Predictors of events were established by univariate analysis and variables with P<.1 were included in the Cox multivariate analysis and expressed as hazar ratio (HR). The cumulative incidence of events was estimated by the Kaplan-Meier method, and compared using the log-rank test. The SPSS Statistics 17 program was used. Statistical significance was set at P<.05.
Baseline characteristics and findings of the cardiac innervation study are shown in the Table. There was a predominance of male patients, who were relatively young and had limited comorbidities. The etiology of LVD was ischemic, as is usually the case in primary prevention of sudden death. Eighteen events were recorded during a mean follow-up of 12.9 (8.6) months: 2 deaths (1 sudden death and 1 death due to heart failure), 7 hospitalizations due to heart failure, 7 appropriate implantable cardioverter defibrillator shocks, and 1 acute myocardial infarction.
Baseline Characteristics of the Overall Sample and According to Whether Major Cardiac Events Occurred
| Total number of patients (n=47) | Patients with events (n=18) | Patients without events (n=29) | P | |
| Male | 34 (72.3) | 12 (66.7) | 22 (75.4) | .493 |
| Age, years | 63.4±9.8 | 65.2±9.8 | 62.2±9.8 | .319 |
| Diabetes mellitus | 28 (61) | 12 (66) | 18 (62) | .518 |
| QRS, ms | 119.8±38.9 | 134.4±43.1 | 109.7±33.0 | .037 |
| Ischemic heart disease | 31 (62) | 12 (67) | 19 (65) | .869 |
| Creatinine, mg/dL | 1.16±0.6 | 1.41±0.8 | 0.99±0.3 | .052 |
| Hemoglobin, mg/dL | 12.9±2.0 | 12.6±2.0 | 13.1±1.0 | .382 |
| BNP, pg/nL | 1087.4±776.6 | 1134.4±823.8 | 1040.4±773.3 | .806 |
| Medication | ||||
| ACE inhibitors or ARB | 44 (94) | 15 (83) | 29 (100) | .051 |
| Beta-blockers | 47 (100) | 18 (100) | 29 (100) | 1 |
| Diuretics | 41 (87) | 18 (100) | 23 (82) | .243 |
| Antialdosterones | 31 (66) | 13 (72) | 18 (62) | .475 |
| Cardiac magnetic resonance imaging | ||||
| LVEF, % | 24.9±9.0 | 26.0±10.8 | 24.4±8.4 | .650 |
| LVEDV, mL/m2 | 136.9±43.7 | 137.5±28.4 | 136.7±49.0 | .961 |
| LVESV, mL/m2 | 104.7±42.5 | 102.9±30.6 | 105.5±47.0 | .874 |
| LGU present | 40 (85.1) | 17 (94) | 23 (79) | .161 |
| 123I-MIBG | ||||
| Early HMR | 1.48±0.22 | 1.42±0.19 | 1.53±0.24 | .086 |
| Late HMR | 1.33±0.20 | 1.27±0.13 | 1.37±0.23 | .049 |
| Washout index, % | 38.60±21.79 | 38.39±23.91 | 38.3±20.8 | .911 |
| Late HMR=1.38 | 27 (57) | 15 (88) | 12 (41) | .005 |
123I-MIBG, 123I-metaiodobenzylguanidine; ACE, angiotensin-converting enzyme; ARB: angiotensin receptor blocker; BNP, brain natriuretic peptide; HMR, heart-to-mediastinum ratio; LGU, late gadolinium uptake; LVEDV, left ventricular end diastolic volume; LVEF, left ventricular ejection fraction; LVESV, left ventricular end systolic volume.
Data expressed as percentage, No. (%), or mean±SD.
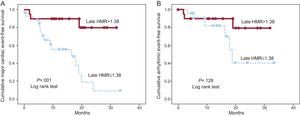
The sample was divided into 2 groups according to the incidence of events. The groups had comparable pharmacological treatment, LVD etiology, presence of late gadolinium enhancement, and left ventricular ejection fraction quantified by cardiac MRI. However, the QRS interval was significantly greater in patients with events. With regard to the findings of cardiac innervation, markedly pathologic HMR values were observed (<1.20, 15 patients; 1.20-1.40, 13 patients; 1.40-1.60, 15 patients;>1.60, 4 patients) and only 1 patient had a normal (>1.80) value. The patients with events had a significantly lower late HMR (1.27 [0.13] vs 1.37 [0.23]; P=.049). The multivariate analysis included QRS interval, creatinine levels, treatment with angiotensin converting enzyme inhibitors/angiotensin II receptor antagonists, and early and late HMR<1.38 (median). An association was observed between late HMR=1.38 (HR=5.19; 95% confidence interval [95%CI], 1.4-19.6; P=.015) and creatinine levels (HR=3.84; 95%CI, 1.8-8.4; P=.001) and an increased risk of experiencing an event. When only arrhythmic events were analyzed, no significant differences were observed in any of the variables. The Figure shows the survival curves for cardiac events and arrhythmic events, stratified using the median value of late HMR (log-rank test, P=.001 and P=.128, respectively).
The results of our study show a marked deterioration in cardiac innervation, as assessed by 123I-MIGB scintigraphy, in patients with severe LVD and indication for implantable cardioverter defibrillator. Moreover, this deterioration was more marked than that reported in previous studies.3–6 In fact, only 5 of the 47 patients had late HMR>1.6 (cut-off point for poor prognosis found in the ADMIRE study4). Even in this setting, this technique manages to identify high-risk patients and could improve noninvasive prognostic stratification, thereby assisting in decision-making.
We recognize the limitations inherent in this design; the study was observational with a limited sample size and a short follow-up period. The study forms part of a larger project in which the combined information provided by 123I-MIGB scintigraphy and cardiac MRI will be assessed. The results presented here should therefore be considered as preliminary.
FUNDINGInstituto de Salud Carlos III, Health Research Fund (PI 10/01112), Medical Research Grant 2010 Fundación grupo ERESA. F. Ridocci-Soriano received funding from the I3 SNS Program for Intensification of Research Activity 2010 and 2012 from the Instituto de Salud Carlos III and the Generalitat Valenciana.
.