The combination of aortic coarctation and dissection is a rare entity, traditionally treated surgically. However, there are still important knowledge gaps. We report the first case in the literature of a patient with postductal aortic coarctation combined with complicated acute type B aortic dissection in which endovascular management was chosen as the first-line treatment, even in the absence of contraindications to surgery.
A 25-year-old man, with no relevant past medical history, presented to the emergency room complaining of transfixing chest pain. A significant difference between blood pressure in the upper and lower extremities (160/90mmHg in the right upper extremity and 110/70mmHg in right lower extremity) was noticed and the intensity of the femoral pulses was diminished. The pulse was regular at 85 beats /min, oxygen saturation was 95%, and a soft diastolic murmur in the second intercostal space was heard. An electrocardiogram showed no abnormalities and chest radiography revealed mediastinum widening.
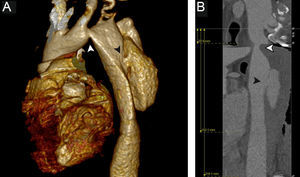
An urgent thoracic computed tomography angiography exhibited an aortic arch coarctation that originated distal to the origin of the left subclavian artery, with an 8-mm minimal diameter and type B aortic dissection immediately after coarctation, which extended to the vertebral level D11, about 4cm above the celiac trunk, with a maximum dilation of 42mm. All the aortic branches remained patent. An echocardiogram confirmed the findings and showed a transcoarctation pressure gradient of 39mmHg, as well as mild aortic regurgitation and preserved left ventricular systolic function.
Given the presence of an uncomplicated acute type B aortic dissection, medical management was provided through antihypertensive drugs and morphine. After 48hours of intensive medical treatment, uninterrupted chest pain and refractory arterial hypertension persisted. A new computed tomography angiography showed an increase of aortic dilation to 65mm (Figure 1). Given the unfavorable clinical course, we decided to perform emergent surgery.
The correction of aortic dissection was prioritized and therefore endovascular treatment was chosen to minimize the risk of ischemic complications. Left percutaneous access and right groin dissection were performed. A transesophageal echocardiogram was performed to locate the true lumen and a Terumo hydrophilic standard guide was placed on the right side. The use of an MP 5-F catheter allowed its passage through the coarctation area. The procedure was repeated on the left side with subsequent placement of a 5-F pigtail catheter.
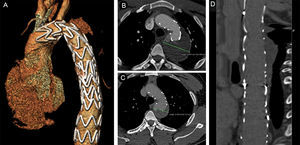
Angiography was performed and 2 thoracic endoprosthesis Relay Plus of 28×28×155mm and 34×34×100mm were placed overlapping, covering the left subclavian artery up to 3cm above the celiac trunk. Subsequently, the coarctation area was dilated with a Reliant balloon, with a satisfactory result (Figure 2A), lowering the pressure gradient to 19mmHg. It was decided not to prevent type II endoleaks by embolisation of collateral circulation between the intercostal branches and left subclavian artery because of the high risk of spinal cord ischemia.
The postoperative course was satisfactory and the patient remains asymptomatic to date. Computed tomography angiography was performed at 1 (Figure 2B) and 6 months (Figure 2C and 2D) of follow-up and a reduction in the diameter of the aneurysm was noted. A type II endoleak from a right intercostal branch, drained through 2 left intercostal arteries, was observed in both tests. We decided to opt for conservative management.
Aortic coarctation represents 5% to 7% of congenital heart disease and usually presents as an isolated narrowing of the juxta-ductal aorta. Current clinical practice guidelines recommend stenting as the first-choice treatment in patients with native aortic coarctation and appropriate anatomy.1 In this regard, the routine use of computed tomography scans has significantly improved treatment decisions in these patients.2
Aortic dissection in the context of an aortic coarctation is a rare entity, with Stanford type A dissection being more common, since elevated blood pressure before the coarctation and progressive aortic dilation are postulated as being the causes of dissection. This combination should be treated surgically. Nevertheless, co-occurrence with type B dissection is even less frequently reported, probably due to low intra-aortic pressure distally to the coarctation.
It is well established that the treatment of uncomplicated type B dissection should be eminently conservative except when complications occur. In these cases, thoracic endovascular aortic repair is preferable if there is feasible vascular anatomy. Open surgery is associated with more procedure-related complications, such as spinal cord ischemia, stroke, mesenteric ischemia, or acute renal failure.1,3
Currently, the joint management of these 2 entities is not well established. We reviewed the existing literature and found few case reports of patients with type B aortic dissection complicating a coarctation; most of these patients were treated surgically,4 but with the risks inherent to open surgical repair. However, the successful completion of a percutaneous approach has been reported in a single patient who persistently refused surgery.5
Our case poses the problem of the optimal management of type B aortic dissection complicating a pre-existing coarctation and suggests that the percutaneous approach is a valid option, even as first-line therapy.