Ablation of ventricular tachycardia (VT) is a procedure that is becoming increasingly more widespread in clinical practice.1 It is estimated that 12% to 17% of cases of VT are of myocardial and subepicardial origin, which is a more common substrate in nonischemic heart disease.2 Rhythmia (Boston Scientific; Marlborough, Massachusetts, United States) is a new nonfluoroscopic navigation system able to generate high-density maps combining a steerable 64-electrode catheter (IntellaMap Orion; Boston Scientific) with software able to automatically capture the recorded electrograms. Given the novelty of the system, experience with this catheter for epicardial mapping is very limited,3 and no information has been published on the outcomes and complications of VT ablation guided by the Rhythmia system.
We present the case of a 56-year-old physician who was an endurance sports enthusiast. He started to experience frequent episodes of palpitations, generally triggered by exercise, and accompanied by nausea. On exercise testing, regular sustained broad QRS tachycardia was induced with right bundle branch block and left superior axis morphology. In the 24-hour Holter recording, 80 episodes of the same tachycardia were detected. The results of both echocardiography and coronary angiography were normal, and diagnosis of VT was confirmed in an electrophysiology study. On magnetic resonance imaging, a 30×7-mm area of gadolinium enhancement was observed between the myocardium and subepicardium of the inferior wall of the left ventricle.
The patient remained symptomatic despite treatment with beta-blockers and was therefore referred to our center for percutaneous ablation.
At rest, he had ventricular extrasystoles and episodes of VT. In view of the information from magnetic resonance imaging, it was decided to perform endocardial and epicardial mapping with the IntellaMap Orion catheter and the Rhythmia system.
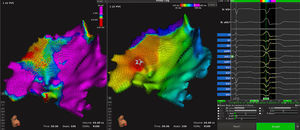
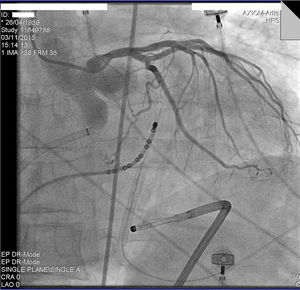
Using percutaneous access, the Orion catheter was introduced into the pericardium through an Agilis steerable sheath. Voltage and activation mapping of the spontaneous tachyarrhythmias was performed. The system automatically selected the appropriate beats for inclusion in the map and only included those with a QRS correlation>90% during the expiratory phase of the respiratory cycle. Voltages>0.5mV were considered normal and those<0.3mV were considered low. A 9180-point map was generated in 26minutes. The map only included extrasystoles and episodes of VT coinciding with clinical tachycardia (Figure 1 and Video 1 of the supplementary material). The site of earliest activation (32ms before onset of QRS) was located on the inferior wall of the left ventricle, close to the ventricular septum, and showed a local single-lead QS-type electrogram. Coronary angiography was performed, which ruled out the presence of major arteries in the vicinity (Figure 2). Radiofrequency pulses were applied with an irrigated-tip ablation catheter. The arrhythmias were temporarily suppressed but recurred after several minutes had elapsed. The ablation catheter was introduced via transeptal access to the endocardial point coinciding with the epicardial map. A single radiofrequency pulse applied at this site definitively suppressed the arrhythmia (Figure 1 of the supplementary material). After 30minutes without spontaneous arrhythmias, isoproterenol was infused intravenously and the VT induction protocol was followed, without inducing any arrhythmias (Figure 2 of the supplementary material). The only complication was pericarditis without significant pericardial effusion, which resolved with anti-inflammatory treatment. After 9 months of follow-up, the patient was asymptomatic and free of arrhythmias.
Epicardial voltage maps (left panel) and activation maps (right panel) of the inferior wall of the left ventricle from a left anterosuperior view. At an earlier time point, an area of low voltage and activation is observed in the inferior part of the left ventricle (star in the middle panel), corresponding to the origin of the ventricular tachycardias. The right panel illustrates how the automatic algorithm correctly samples a clinical extrasystole.
This is a case of VT originating from a ventricular myocardial-epicardial scar. The tachycardia was treated effectively by focal ablation guided by epicardial mapping with an Orion catheter. In the case presented, the performance of the system was notable, reflecting the ease with which the multipolar catheter could be steered in the pericardial space and the precision of ventricular activation mapping. In this case, the algorithm for recognition of QRS of the target VT was very specific in, even during mechanical induction of multiple extrasystoles, which the system rejected systematically.
One of the specific characteristics of the system during epicardial mapping, in contrast to conventional catheters, is that the Orion catheter electrodes are electronically printed on the splines of the basket such that, instead of showing a 2-dimensional epicardial map, a virtual space is generated. Therefore, the epicardial map generated with the Orion catheter should always be visualized from inside the virtual cavity. If, as often occurs, the external face of the map is visualized, false areas of low voltage are observed, arising because only electrograms recorded with electrodes that probed the parietal pericardium are selected (Video 2 of the supplementary material).
In conclusion, in the opinion of the authors, epicardial mapping with this new system is possible and offers an electroanatomical map with a very high point density.