Heart failure (HF) has become an important health problem in western countries given its high prevalence, incidence, and mortality.1 Several drugs and nonpharmacological interventions (for example, cardiac resynchronization therapy and implantable cardioverter-defibrillators) have been shown to improve prognosis, but only in patients with impaired systolic function. These findings are reflected in the clinical guidelines, such as the 2012 European Society of Cardiology guidelines,2,3 which recommend that all patients with symptomatic systolic HF should receive diuretics, angiotensin conversion enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), beta-blockers, and mineralocorticoid receptor antagonists (MRAs). Patients with a heart rate greater than 70 beats per minute in sinus rhythm should also receive ivabradine. In everyday practice, however, these drugs are not as widely used as recommended.4,5 The low rate of use may, in part, be explained because population-based studies include patients with HF with no systolic impairment (who account for 35%-50% of all cases) in addition to those with systolic HF, thereby confounding the results on adherence to the recommendations of the guidelines. The information on actual adherence should be derived from registries that only and specifically include patients with systolic HF.
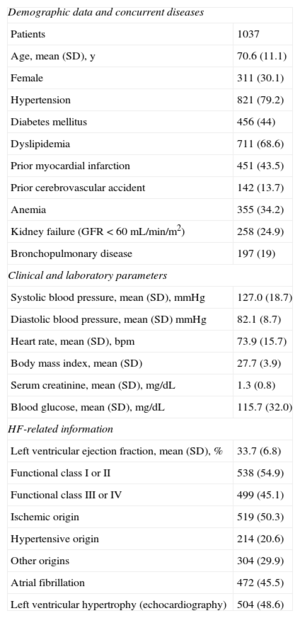
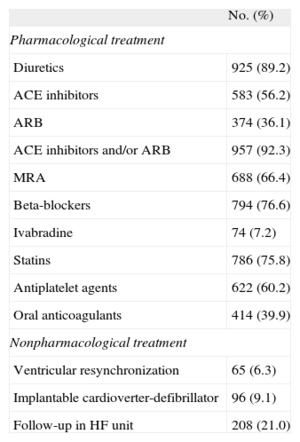
The VIDA-IC was a prospective study conducted by 115 specialists (cardiologists or internal medicine specialists) throughout Spain; each investigator aimed to enroll 10 consecutive patients with HF and ejection fraction < 40%, seen in an outpatient clinic, and with no history of admission for HF in the month prior to the baseline visit. In total, 1037 patients with valid data were recruited between October 2011 and January 2012. Cardiologists recruited 63% of the patients and internal medicine specialists recruited the remaining 37%. The study was approved by the ethics committee of the Hospital del Mar, Barcelona, Spain. Table 1 shows the demographic, clinical, and functional characteristics of the patients. The mean (standard deviation) age was 70.6 (11.1) years and 30% were women. In total, 21% of patients were followed in specific HF units. The mean left ventricular ejection fraction was 33.7% (6.8%). HF was predominantly of ischemic origin and >45% of patients had atrial fibrillation. Approximately half the patients were in functional class III-IV on inclusion and 83% had been admitted to hospital previously for HF. As reflected in Table 1, there was a high prevalence of concurrent diseases in our patients. More than 92% were receiving an ACE inhibitor or an ARB, 76.6% were receiving beta-blockers, and 66.4% were receiving an MRA (Table 2). Only 7.2% were receiving ivabradine and the percentage of patients who underwent cardiac resynchronization therapy or implantable cardioverter-defibrillator placement was low (6.3% and 9.1%, respectively). Only 55% of the patients were receiving optimal pharmacological treatment, defined as joint administration of ACE inhibitors or ARBs, beta-blockers, and MRAs. For the remaining 45%, failure to prescribe drugs from all 3 therapeutic groups was not due to contraindications, as absolute contraindications were only present in 3.2% for beta-blockers and 5.6% for MRAs.
Demographic, Clinical, and Functional Characteristics of the Study Patients
| Demographic data and concurrent diseases | |
| Patients | 1037 |
| Age, mean (SD), y | 70.6 (11.1) |
| Female | 311 (30.1) |
| Hypertension | 821 (79.2) |
| Diabetes mellitus | 456 (44) |
| Dyslipidemia | 711 (68.6) |
| Prior myocardial infarction | 451 (43.5) |
| Prior cerebrovascular accident | 142 (13.7) |
| Anemia | 355 (34.2) |
| Kidney failure (GFR<60 mL/min/m2) | 258 (24.9) |
| Bronchopulmonary disease | 197 (19) |
| Clinical and laboratory parameters | |
| Systolic blood pressure, mean (SD), mmHg | 127.0 (18.7) |
| Diastolic blood pressure, mean (SD) mmHg | 82.1 (8.7) |
| Heart rate, mean (SD), bpm | 73.9 (15.7) |
| Body mass index, mean (SD) | 27.7 (3.9) |
| Serum creatinine, mean (SD), mg/dL | 1.3 (0.8) |
| Blood glucose, mean (SD), mg/dL | 115.7 (32.0) |
| HF-related information | |
| Left ventricular ejection fraction, mean (SD), % | 33.7 (6.8) |
| Functional class I or II | 538 (54.9) |
| Functional class III or IV | 499 (45.1) |
| Ischemic origin | 519 (50.3) |
| Hypertensive origin | 214 (20.6) |
| Other origins | 304 (29.9) |
| Atrial fibrillation | 472 (45.5) |
| Left ventricular hypertrophy (echocardiography) | 504 (48.6) |
GFR, glomerular filtration rate; HF, heart failure; SD, standard deviation.
Data expressed as mean (standard deviation) or No. (%).
Treatments Received by Study Patients (n=1037)
| No. (%) | |
| Pharmacological treatment | |
| Diuretics | 925 (89.2) |
| ACE inhibitors | 583 (56.2) |
| ARB | 374 (36.1) |
| ACE inhibitors and/or ARB | 957 (92.3) |
| MRA | 688 (66.4) |
| Beta-blockers | 794 (76.6) |
| Ivabradine | 74 (7.2) |
| Statins | 786 (75.8) |
| Antiplatelet agents | 622 (60.2) |
| Oral anticoagulants | 414 (39.9) |
| Nonpharmacological treatment | |
| Ventricular resynchronization | 65 (6.3) |
| Implantable cardioverter-defibrillator | 96 (9.1) |
| Follow-up in HF unit | 208 (21.0) |
ACE, angiotensin converter enzyme; ARB, angiotensin receptor blockers; HF, heart failure; MRA, mineralocorticoid receptor antagonist.
These results, collected from a recent, large, multicenter sample of patients in real-life clinical practice in Spain, show underuse of recommended treatments despite the evidence and clear recommendations in the clinical practice guidelines. The percentage of patients who receive ACE inhibitors or ARBs is high and prescription rates for beta-blockers and MRAs is respectable, in the latter case probably because of the results of the EMPHASIS–HF study with eplerenone.6 Nevertheless, almost half the patients did not receive the optimal recommended treatment (ACE inhibitors or ARBs, beta-blockers, and MRA). Use of ivabradine is lower still, even when the mean heart rate exceeds 70 beats per minute. The recommendation for use of ivabradine is the most recent, and this may have had some bearing on the low uptake. In the pilot registry study for HF,4 published in 2010, prescription of ACE inhibitors or ARBs to patients with systolic HF was 91%; the percentage receiving beta-blockers was greater (87%) and the percentage receiving MRA was lower (43%) than in the VIDA-IC study. In the most recent long-term study,5 the rate of use of these 3 therapeutic classes was 92%, 92%, and 67%, respectively. We can conclude that, despite advances in recent years in the treatment of systolic HF, there is still plenty of room for improvement in our patients, particularly in terms of use of beta-blockers, MRA, and ivabradine.
CONFLICTS OF INTERESTPfizer S.L.U. is the sponsor of the VIDA-IC study and provided funding. The authors have received honoraria from Pfizer S.L.U. for the design of the study and the drafting and review of this article.