The percutaneous implantation of prosthetic heart valves in degenerated bioprostheses in different positions has provided an alternative to surgery in patients with congenital or acquired heart disease who are at high surgical risk. There is little experience with percutaneous implantation of prostheses in tricuspid position. We report the case of a patient with a stenotic tricuspid bioprosthesis who was treated with a percutaneously implanted prosthesis. To our knowledge, this was the first time this intervention was performed in Spain.
The patient was a 38-year-old man, diagnosed as having Ebstein anomaly with an atrial septal defect, who had undergone tricuspid valve replacement by a 31-mm Biocor bioprosthesis and atrial septal defect closure at the age of 23 years. During the postoperative period, he developed acute thrombosis that was resolved with fibrinolysis and had another episode 6 months later coinciding with the discontinuation of anticoagulation therapy. He was found to have advanced atrioventricular block and underwent implantation of a DDD pacemaker with an intracavitary atrial lead and an epicardial ventricular lead. Over the preceding 3 years, he had shown clinical signs of right heart failure that required diuretic therapy. An echocardiogram revealed degenerative changes in the bioprosthesis that were causing marked stenosis (peak gradient, 13mmHg; mean gradient, 9mmHg) with mild regurgitation, in addition to severe right ventricular dysfunction. The patient underwent catheterization, which revealed a tricuspid diastolic pressure gradient of 10mmHg, with a mean right atrial pressure of 14mmHg and a cardiac index of 1.9 L/min/m2. Given the high risk, both valve replacement and surgery to perform the Glenn procedure were ruled out, and he was scheduled for percutaneous prosthesis implantation.
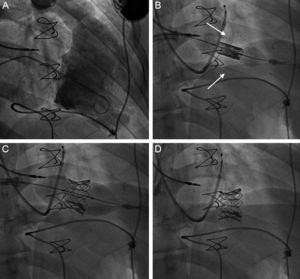
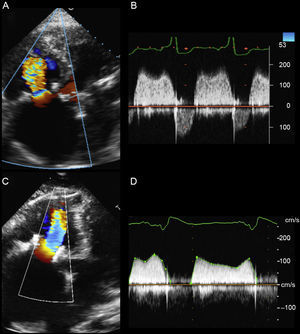
The procedure was carried out with general anesthesia. A right jugular vein approach was employed to implant a temporary pacemaker at the level of the coronary sinus for rapid pacing during the valve implantation. Using a left femoral venous approach because the right femoral vein was occluded, the tricuspid bioprosthesis was crossed with a balloon catheter, and a high-support guide wire was introduced at the level of the right ventricle. Once the vein had been prepared with several 12-Fr to 20-Fr dilators, a 20-Fr introducer was placed. Subsequently, with no predilation, we implanted a 29-mm Edwards-SAPIEN XT prosthesis (Edwards Lifesciences; Irvine, California, United States), mounted in the direction contrary to the usual manner (implantation in aortic position via femoral access), over the NovaFlex+ release system (Edwards Lifesciences) and within the degenerated bioprosthesis. There were no technical difficulties either along the delivery route or at the point where the prosthesis crossed over the bioprosthesis. As a reference for the implantation, we used the radiopaque annulus of the bioprosthesis in right anterior oblique projection, where it remained perpendicular. The balloon was slowly inflated with rapid pacing, and nearly the entire percutaneously implanted prosthesis was placed in the ventricular part of the annulus of the bioprosthesis to ensure that this new prosthesis covered the degenerated leaflets of the first device (Figure 1). There was an immediate deterioration in right ventricular function, probably related to the rapid pacing and lengthy procedure employed for prosthesis implantation. An echocardiogram performed 24hours later showed recovery of right ventricular function and normal function of the prosthesis (peak gradient, 6mmHg; mean gradient, 3.5mmHg) (Figure 2). One month later, the patient showed no signs of right heart failure and was being treated indefinitely with acenocoumarol (which he previously had been taking) and acetylsalicylic acid, in addition to a 3-month regimen of clopidogrel.
A: Right ventriculography showing a dilated chamber with a degenerated bioprosthesis and mild tricuspid regurgitation. B: Edwards-SAPIEN prosthesis implantation with placement of the largest portion toward the ventricular side of the annulus (arrows). C: Complete inflation of the balloon with the prosthesis. D: Final fluoroscopy with the implanted prosthesis.
A: Baseline transthoracic echocardiography in 4-chamber projection, with accelerated flow over the degenerated bioprosthesis. B: Baseline peak gradient of 13mmHg and mean gradient of 9mmHg, according to continuous Doppler. C: 24-hour, 4-chamber transthoracic echocardiography 24hours after implantation. D: Peak gradient of 6mmHg and mean gradient of 3.5mmHg, according to continuous Doppler.
The choice of the 29-mm Edwards-SAPIEN model was based on the size of the degenerated bioprosthesis, which measured 31mm and had an internal diameter of 29mm. The alternative prosthetic valve for percutaneous implantation in tricuspid position is the Melody (Medtronic Inc., Minnesota, United States), but it was inappropriate because the maximum available diameter is 22mm, which would have been too small for the case we report here. There is little experience with the percutaneous implantation of an Edwards-SAPIEN prosthesis over a bioprosthesis in tricuspid position, there being around 20 published cases. In most of them, placement was achieved using a direct transatrial or a transjugular approach, whereas there have only been 6 cases involving femoral access. The transatrial and transjugular approaches enable direct access to the tricuspid valve, making the procedure simpler to perform. However, the inconvenience of the transatrial approach is that it requires thoracotomy, and the drawback to the transjugular approach is the need for introducers of a larger gauge, as this technique requires a transapical delivery system, which, for a 29-mm prosthesis, would involve a 26-Fr sheath. This, in turn, would necessitate surgical closure of the jugular vein. In the 6 reported cases of femoral access, the bioprosthesis was previously dilated. This is the first report of a case of direct implantation with no predilation, via femoral access. The risk of prosthesis migration during implantation is probably lower when predilation is not performed, and the material within the degenerated bioprosthesis is usually friable, and thus is usually easy to cross through. Moreover, embolization of this material is reduced with direct implantation.1
This case demonstrates the feasibility of implanting an Edwards-SAPIEN prosthesis at the level of a degenerated tricuspid bioprosthesis using the femoral approach and without predilation. A larger number of cases and follow-up over several years will be necessary to confirm the utility of this new strategy for valve therapy.
We thank André Oliveira for his assistance during prosthesis implantation.