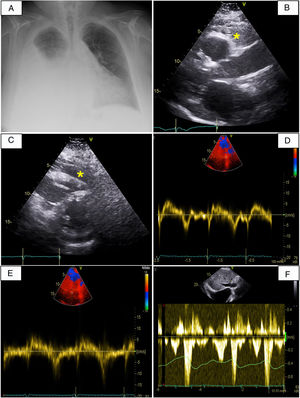
We present the case of a 73-year-old hypertensive, obese woman who presented with worsening functional class and dyspnea on minimal exertion. She had a history of permanent atrial fibrillation and numerous admissions for congestive heart failure with preserved left ventricular ejection fraction. Physical examination showed signs of congestion and a chest radiograph showed bilateral, predominantly right-sided, pleural effusion (figure 1A). The patient was admitted to the cardiology ward.
A, Posteroanterior chest radiograph showing pleural effusion in the right hemithorax. B and C, Two-dimensional parasternal transthoracic echocardiogram in short-axis (B) and long-axis (C) views showing abundant epicardial fat (asterisks). D and E, Tissue Doppler imaging of the lateral (D) and medial (E) mitral annulus showing annulus reversus with a longer medial e’ (15cm/s) than lateral e’ (8cm/s). F, Diastolic flow reversal in the hepatic veins on Doppler echocardiogram.
As this was the fifth time the patient had been admitted for pleural effusion with marked right-side predominance in the past year, it was decided to perform a thoracentesis, which showed transudative pleural fluid. A transthoracic echocardiogram (figure 1B,C) showed signs of pericardial constriction with a markedly dilated inferior vena cava that did not collapse with inspiration, apparent pericardial thickening with septal bounce (video 1 of the supplementary data), annulus reversus (lateral e’ < medial e’) (figure 1D,E), and hepatic vein expiratory flow reversal (figure 1F). The patient also had severe tricuspid regurgitation with normal valvular and annulus morphology, allowing estimation of a pulmonary artery systolic pressure of 50mmHg.
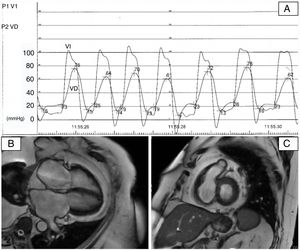
Based on these findings, it was decided to perform right heart catheterization, which demonstrated postcapillary pulmonary hypertension (mean pulmonary artery pressure of 40mmHg and pulmonary capillary pressure of 27mmHg) and a left ventricular dip and plateau pattern with elevation and equalization of end-diastolic pressures in both ventricles. These signs were all consistent with a diagnosis of constrictive pericarditis (figure 2A). The only relevant finding on a subsequent cardiac magnetic resonance imaging scan was abundant epicardial and mediastinal fat (without evident pericardial thickening) and signs of ventricular interdependence (figure 2B,C and video 2 of the supplementary data).
A, Cardiac catheterization showing a left ventricular dip and plateau pattern with elevation and equalization of end-diastolic pressures in both ventricles. B and C, Steady-state free precession cardiac magnetic resonance imaging 4-chamber view (B) and short-axis (C) showing abundant epicardial fat accumulation.
Given the striking constrictive physiology observed and the patient's history, it was decided to perform a pericardiectomy to remove fat. The outcome was favorable and the patient did not develop any complications and was discharged after 7 days. The postoperative echocardiogram showed moderate tricuspid regurgitation and decreased expression of findings indicative of elevated end-diastolic pressures in the right cavities (video 3 of the supplementary data). Follow-up outpatient radiographs showed minimal right-sided pleural effusion and no build-up of fluid since the surgery. The patient did not experience any new episodes or require hospitalization during 1 year of follow-up and remains in New York Heart Association class I.
Epicardial fat is a unique fat compartment located between the myocardium and the visceral layer of the pericardium. It accounts for approximately 20% of total heart weight and under physiological conditions covers almost 80% of the surface of the heart. Epicardial fat thickness varies according to sex and body mass index and is greater in men and obese people.
Although epicardial fat has beneficial effects—it protects the myocardium from hypothermia damage, for example, and acts as an energy reservoir—a number of potentially deleterious effects have been described in recent years, with epicardial fat appearing to be an important factor in inflammation, atherosclerosis, and insulin resistance. In addition, epicardial fat thickness has been linked to the development of atrial fibrillation,1 and larger volumes have been observed in patients with heart failure and preserved left ventricular ejection fraction compared with comorbidity-matched controls.2
Little has been reported on the potentially deleterious effects of very abundant epicardial fat, but it could affect myocardial contractility by favoring constrictive physiology and acting as a rigid, thickened, pericardium. In our review of the literature, we found a case of a 59-year-old woman with extensive epicardial fat associated with constrictive pericarditis and heart failure who died before surgery could be performed.3 Another more recent report described the case of a patient with calcified epicardial fat necrosis causing epicardial constriction.4
Constrictive pericarditis is characterized by pathologic pericardial rigidity and thickening resulting in impaired diastolic filling and, as a consequence, elevated systemic venous pressures.5 Patients develop predominantly right-sided heart failure, which classically manifests as systemic venous congestion and decreased functional capacity.
As occurred in our case, a Doppler echocardiogram can show some signs of constrictive physiology and impaired ventricular filling, such as an early diastolic notch on the interventricular septal echocardiogram in mode M, in addition to prominent diastolic flow in the inferior vena cava and the hepatic veins, which show flow reversal with expiration. Characteristic cardiac catheterization findings, also observed in our case, include elevation and equalization of diastolic pressures in both ventricles (the classic dip and plateau or square root sign).
Constrictive physiology due to epicardial fat should be suspected in patients with compatible clinical and other diagnostic findings.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2020.04.022