Single measurements of cardiac biomarkers have shown predictive value in asymptomatic severe aortic stenosis (SAS). Our group has previously shown that a baseline level of highly sensitive troponin T (hsTnT) was associated with a 10-fold greater risk of events, and that incorporation of hsTnT into a model that included age, sex, aortic regurgitation ≥ 2+, left atrial volume index, diastolic dysfunction of ≥ 2, mean aortic gradient, N-terminal pro-B-type natriuretic peptide (NT-proBNP) and longitudinal strain significantly increased discrimination and adequately reclassified 43% of patients1; nevertheless, dynamic changes of these biomarkers over time and their association with outcomes remain unknown.
To determine whether increases in biomarkers over time might improve event risk prediction in asymptomatic SAS, we examined the values of repeat NT-proBNP and hsTnT measurements at baseline and 6 months.
We prospectively studied 79 consecutive patients who were admitted to a heart valve clinic with asymptomatic SAS from January 2014 to June 2018. Two patient groups were established, based on whether they experienced events (n=25) or no events (n=54) within 1 year. Events were defined as the presence of cardiovascular death, SAS-related clinical symptoms, hospital admission due to cardiac causes, or an indication for aortic valve replacement.
The mean age was 74± 9 years; 30% had diabetes, 77% had dyslipidemia, 3 had clinically known ischemic heart disease, and only 1 had a history of myocardial infarction. However, on coronary angiography, 16 of the 45 patients examined had significant coronary stenosis (10 in 1 vessel, 4 in 2 vessels, 2 in 3 vessels, and 2 left main disease). Patients with severe aortic regurgitation were excluded. The mean±standard deviation echocardiography values were as follows: maximum aortic velocity, 4.2±0.28; aortic gradient, 48.2±7.6mmHg; aortic valve area, 0.78±0.11cm2; left ventricular ejection fraction, 68±5.6%; left atrial indexed volume, 40.3±13.0mL/m2. Aortic regurgitation ≥ 2 was present in 17% of patients. The median (Q1-Q3) baseline and 6-month NT-proBNP levels were 294 [139-656] and 350 [174-875] ng/L, respectively. The median (Q1-Q3) baseline and 6-month hsTnT levels were 13.0 [8.6-18.0] and 14.1 [8.9-23.2] ng/L, respectively.
The events occurring during the first year of follow-up were as follows: 16 patients developed symptoms (all had heart failure, 1 had angina and 2 had syncope, of whom 1 required hospital admission). Aortic replacement was indicated in 9 patients due to the results of the echocardiographic stress test, in 2 due to a drop in left ventricular ejection fraction, and based on symptoms in the remaining patients. Indications were never based on biomarker data. The clinician responsible for patient management and therapeutic decision-making was blinded to hsTnT values but not to NT-proBNP values.
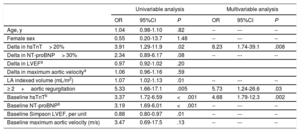
On univariable analysis, several baseline echocardiographic data, baseline levels of both biomarkers and a> 20% change in hsTnT dynamics at 6 months (ΔhsTnT> 20%) were significantly associated with the presence of events (table 1). We performed a multivariable binomial logistic regression analysis (backward stepwise conditional) to identify predictors for the risk of events at 1 year, including age, sex and variables with a value <0.10 in the univariable analyses, and baseline maximum aortic velocity, considered clinically relevant for the addressed valvular disease. We found that a ΔhsTnT> 20% from baseline to 6 months was an independent predictor of 1-year events (odds ratio, 8.23; 95% confidence interval [95%CI], 1.74-39.1; P=.008), together with aortic regurgitation ≥ 2+(P=.03) and baseline hsTnT (P=.002) (table 1). In a sensitivity analysis, only patients with clinical events were assessed and, in a multivariable binomial logistic regression analysis (backward stepwise conditional) including age, sex, and biomarker data (both baseline and dynamic changes) a ΔhsTnT> 20% remained significantly associated with such events (hazard ratio, 5.31; 95%CI, 1.27-22.2; P=.02). Thus, we recommend that measuring the hsTnT biomarker at predefined intervals of 6 months could improve asymptomatic SAS prediction and decision-making.
Univariable and multivariable (conditional backward stepwise) binomial logistic regression analysis for the risk of events at 1 year
| Univariable analysis | Multivariable analysis | |||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| Age, y | 1.04 | 0.98-1.10 | .82 | -- | --- | -- |
| Female sex | 0.55 | 0.20-13.7 | 1.48 | -- | --- | -- |
| Delta in hsTnT> 20% | 3.91 | 1.29-11.9 | .02 | 8.23 | 1.74-39.1 | .008 |
| Delta in NT-proBNP> 30% | 2.34 | 0.89-6.17 | .08 | -- | --- | -- |
| Delta in LVEFa | 0.97 | 0.92-1.02 | .20 | |||
| Delta in maximum aortic velocitya | 1.06 | 0.96-1.16 | .59 | |||
| LA indexed volume (mL/m2) | 1.07 | 1.02-1.13 | .01 | -- | --- | -- |
| ≥ 2+aortic regurgitation | 5.33 | 1.66-17.1 | .005 | 5.73 | 1.24-26.6 | .03 |
| Baseline hsTnTb | 3.37 | 1.72-6.59 | <.001 | 4.68 | 1.79-12.3 | .002 |
| Baseline NT-proBNPb | 3.19 | 1.69-6.01 | <.001 | -- | --- | -- |
| Baseline Simpson LVEF, per unit | 0.88 | 0.80-0.97 | .01 | -- | --- | -- |
| Baseline maximum aortic velocity (m/s) | 3.47 | 0.69-17.5 | .13 | -- | --- | -- |
95%CI, 95% confidence interval; hsTnT, highly sensitive troponin T; LA, left atrium; LVEF, left ventricular ejection fraction; NT-proBNP, N-terminal pro-B-type natriuretic peptide; OR, odds ratio.
These findings are consistent with previous reports demonstrating that the progression of biomarker levels over time might anticipate events in patients with symptomatic SAS. Henry et al.2 found that natriuretic peptide dynamics were valuable in this clinical setting, but did not measure other biomarkers. The present study highlights the value of a myocyte injury biomarker, namely hsTnT, and the limited value of a myocyte stress biomarker, namely NT-proBNP. Indeed, the significant association between ΔhsTnT> 20% from baseline to 6 months and the occurrence of events was independent of classic variables with important predictive value in patients with asymptomatic SAS3 (ie, the maximum aortic velocity, ejection fraction, and NT-proBNP changes), even after adjustment of the regression model with the baseline values of all these variables.
Further studies are needed to validate our finding that hsTnT dynamics could be used to indicate valve replacement before the occurrence of irreversible left ventricular changes. This biological approach is likely to be the next frontier in managing patients with severe SAS.4,5
FUNDINGThe study (EF-S) was supported by a competitive grant from Societat Catalana Cardiologia (2014).
CONFLICTS OF INTERESTA. Bayés-Genís has received lecture honoraria from Roche Diagnostics. The rest of the authors declare no conflicts of interest.