We present a case of acute pericarditis coinciding with a pericardial cyst with atypical location, probably triggered by infection with severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2), which resolved completely after anti-inflammatory treatment. Viral etiology is the most common cause of acute pericarditis.1 Recently, cases of pericarditis after infection with SARS-CoV-2 have been documented.2 In the literature, there are cases of resolution of the pericardial cyst, but none with the atypical location described here.3,4
In May 2020, a 21-year-old man (who gave informed consent for subsequent investigations and authorized this publication), with no past medical history of note, presented to the emergency department with a 12-day history of chest pain suggestive of pericarditis and a fever of 39°C. Six weeks prior, he had experienced symptoms for 1 week of cough, fever, headache, odynophagia, and myalgia, which was diagnosed as “suspected COVID-19” based on close contact with another household member who had a positive reverse-transcriptase polymerase chain reaction (RT-PCR) for SARS-CoV-2. At that point, RT-PCR and serological testing were not performed due to limited availability.
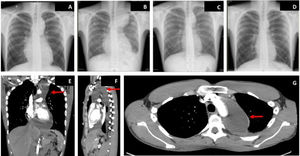
On arrival, blood pressure was 115/80mmHg, heart rate was 110 bpm, baseline oxygen saturations were 95%, and temperature was 37.2°C. On examination, a pericardial rub was noted. Electrocardiogram showed shortened PR interval and diffuse concave ST-segment elevation with normal voltages. Chest X-ray showed marked mediastinal widening (figure 1A) that prompted us to perform urgent computed tomography (CT) to rule out acute aortic syndrome: this showed bilateral pleural effusion and pericardial effusion with substantial extension into the superior aortic pericardial recess, with pericardial enhancement after administration of intravenous contrast (figure 1E-G). The aorta, pulmonary arteries, and lung parenchyma showed no significant abnormalities.
Blood tests revealed raised C-reactive protein (175mg/L) and ferritin (408 ng/mL). Echocardiogram showed the heart chambers had normal size, preserved biventricular systolic function, and diffuse pericardial effusion mainly in the posterolateral area (1.2 cm), with no signs of hemodynamic compromise. Based on a diagnosis of acute pericarditis, treatment was started with aspirin (1 g/8h) and colchicine (1mg/24h).
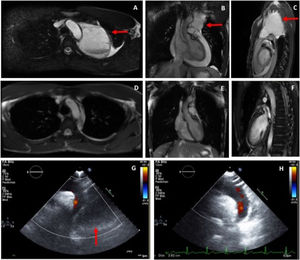
Cardiac magnetic resonance (CMR) was performed and showed, adjacent to the predominantly superior pericardial effusion, a thin-walled cyst in the mediastinum measuring 7.6×7×9.7 cm (figure 2A-C) whose content had a signal intensity higher than that of the pericardial effusion, indicative of higher protein content. On prone sequences, both the pericardial effusion and the pleural fluid displaced anteriorly, while the cyst remained in a posterior position. The findings indicated acute pleuropericarditis with a pericardial cyst of atypical location.
Pericardial cyst (arrows) on cardiac magnetic resonance on axial (A), coronal (B), and sagittal (C) views. Cardiac magnetic resonance at one month post-discharge showing complete resolution; axial (D), coronal (E), and sagittal (F) views. Echocardiogram on suprasternal view on admission (G: with pericardiac cyst, arrow) and at 1 month after resolution (H).
The patient was slow to improve, with persistent chest pain, temperature spikes, increased C-reactive protein up to 329 mg/dL with normal procalcitonin, radiological worsening (figure 1B) and increase in the pericardial effusion (up to 2.2 cm posterolaterally) but without hemodynamic compromise. He was therefore started on intravenous corticosteroids (0.5mg/kg/24h). In the following 48hours, the patient showed clear improvement, both clinically and on blood tests. One week later, echocardiogram no longer showed pericardial effusion, but the pericardial cyst persisted. Markers of myocardial damage were normal throughout. Blood cultures were negative.
An etiological screen was carried out with viral serology, which ruled out acute infection with cytomegalovirus, Epstein-Barr virus, varicella-zoster virus, parvovirus B19, toxoplasmosis, and human immunodeficiency virus. RT-PCR for SARS-CoV-2 and serological levels of IgM and IgG against SARS-CoV-2 were negative. Tumor markers, immunological study, and thyroid-stimulating hormone were normal. Mantoux test was negative.
After improving clinically, on blood tests, and radiologically (figure 1C), the patient was discharged. However, due to the persistence of the pericardial cyst, he was referred to thoracic surgery for assessment for invasive treatment. CMR performed at 1 month showed complete resolution of the pleural effusion, pericardial effusion, and associated cyst (figure 2D-F), making surgical treatment unnecessary.
Pericardial cysts and diverticulae are a rare, benign entity (incidence, 1:100 000) that make up 6% of mediastinal masses.1,5,6 They are usually congenital or, less frequently, are acquired with an inflammatory origin.5 The most common location is at the right cardiophrenic angle (51%-70%), followed by the left cardiophrenic angle (28%-38%); location in the superior mediastinum is unusual.5 They are usually isolated, simple, and measure <5 cm.5 They are generally asymptomatic and found incidentally on routine chest X-ray.5 Other diagnostic techniques are echocardiography, CT, and CMR.5 Large cysts may cause compressive symptoms and may cause serious complications such as cardiac tamponade.5 If symptomatic, the first line of treatment is percutaneous drainage, which has a recurrence rate of 30%; if this happens, surgical resection is required.1
Unlike cysts, pericardial diverticulae freely communicate with the pericardial space, which can be identified by changes in the shape and size with changes in position or with respiration.6 In the case presented here, although some of the CMR projections suggested a degree of connection between the cyst and the pericardial space, there did not appear to be an open communication that allowed passage of fluid. The unchanging size of the pericardial mass with postural changes, the higher intensity of its content compared with the pericardial effusion (characteristic of pericardial cysts6) and its persistence after the pericardial effusion had completely resolved made us lean toward a diagnosis of pericardial cyst.
The increase in the pericardial cyst during the episode of acute pericarditis could be explained by the inflammatory reaction in the pericardial membranes, or due to a potential anatomical continuity. This case illustrates that, in patients with pericardial cysts with an inflammatory component, conservative treatment may be a suitable first choice.
FUNDINGThere was no funding source.
AUTHORS’ CONTRIBUTIONSAll the authors contributed to the writing of this article.
CONFLICTS OF INTERESTThe authors declare that there are no conflicts of interest.