Keywords
INTRODUCTION
Prehypertension is associated with high blood pressure and higher cardiovascular risk, and it should be suggested to prehypertensive patients that they modify their lifestyle in order to help avoid these problems.1-4 "Cardiovascular risk" refers to the probability of developing cardiovascular disease within a determined time, usually 5 or 10 years. The most common methods used for estimating cardiovascular risk are based on the criteria used in the Framingham2,5,6 and SCORE7,8 studies. In addition to pharmacological strategies, making changes in lifestyle can help reduce cardiovascular risk and blood pressure. Positive modifications of lifestyle include increasing physical activity, changes in eating habits, and the elimination of addictions. A number of studies8-11 have shown the effect of such modification on certain components of cardiovascular risk.
The aim of this study was to determine the clinical effectiveness of modifying lifestyle to reduce cardiovascular risk in prehypertensive individuals, and to compare the results obtained with those achieved by the standard management of such patients.
METHODS
This study was an open clinical trial involving prehypertensive individuals who agreed to make lifestyle changes, and a second group of subjects who received standard management at primary health care clinics in Mexico. To be included, subjects of either sex had to be between 30 and 55 years of age, to have a systolic blood pressure of 120-139 mm Hg and a diastolic blood pressure of 80-89 mm Hg, to have no chronic complications, to not be taking oral contraceptives in the case of women patients, and to be receiving no hormonal or other treatment that might modify the blood pressure. Subjects who failed to attend 3 or more exercise sessions (see below) were excluded. The sample size required was estimated taking into account a type I error of 0.05 and a type II error of 0.8. The final study population included 92 patients who were randomly assigned to the experimental or control groups. The researchers responsible for the statistical analysis of the results were blind to the groups to which the different subjects were assigned.
The members of the treatment group undertook a lifestyle modification program for a period of 6 months. Following a nutritional analysis they were assigned a low-sodium, DASH-type diet, the energy provision of which was estimated using the Harris-Benedict formula. Adherence was evaluated via the use of a 24 h record. They also undertook 3-5 sessions per week of aerobic physical exercise (walking, running, swimming) complemented by group sport sessions (soccer, basketball, volleyball, or "cachibol" [a form of volleyball often played by older persons]). Each session lasted 45 min, starting with stretching exercises followed by 30 min of specific exercise and a recovery phase. The physical and aerobic capacity of each subject was determined by the Cooper test and by determining the maximum oxygen consumption (VO2max). Prehypertensive subjects who smoked also attended 6 educational classes.
The members of the control group were managed following the usual recommendations provided by primary health care clinics in Mexico. They received guidelines outlining exercises they should undertake, plus dietetic recommendations. The latter, however, only took into account sodium restriction and energy intake in accordance with ideal weight.
The general change in lifestyle accomplished was assessed using the FANTASTIC questionnaire, which contains 25 questions covering 9 areas including physical activity, nutrition, addictions, and daily activities. The answers are Likert-type with a weighting of 0-5; reliability is 0.8412.
Cardiovascular risk was estimated using the Framingham tables proposed by Wilson et al,2 taking into account age, use of tobacco, the presence of diabetes mellitus, blood pressure, total cholesterol, and level of high density lipoprotein cholesterol. Determinations were made at the start of the study and again at 3 and 6 months. The probability of suffering a cardiac event within 10 years was also calculated.
The analysis of clinical effectiveness took into account the proportion of patients that saw a reduction or increase in their cardiovascular risk, the relative risk (RR), the reduction in relative risk (RRR), the absolute reduction in risk (ARR), and the number of patients who needed treatment (NNT). Differences between the groups were analyzed using the Friedman c2 test and the Mann-Whitney U test.
RESULTS
Thirty eight prehypertensive patients completed the study in the treatment group, as did 43 in the control group. The mean age of the members of the treatment group was 43.97 (7.65) years; in the control group this was 42.56 (7.98) years (P>.05). With the exceptions of blood pressure and sex, the 2 groups were comparable in terms of cardiovascular risk (Table 1).
Initial lifestyle scores (median [range]) were similar in both groups: 62.5 (43-83) in the treatment group, and 65 (33-87) in the control group (P>.05). The intervention increased the median lifestyle score of the members of the treatment group to 80.5 (62-92), whereas that achieved in the control group was 72 (45-86) (P<.05). Three smokers in the treatment group abandoned their habit whereas none did so in the control group.
The physical capacity of the members of the treatment group increased from 1100.53 (267.58) to 1436.18 (318.78) m by the end of the intervention (P<.01), and the VO2max increased from 13.23 (5.95) to 20.69 (7.08) mL/kg/dL (P<.01). Furthermore, all cardiovascular risk factors improved, except for total cholesterol. Systolic blood pressure was reduced from a mean of 133.03 (4.36) to 119 (7.97) mm Hg (P<.05) and diastolic blood pressure was reduced from a mean of 87.58 (2.84) to 76.26 (5.61) mm Hg (P<.05). Finally, the waist measurement of these subjects was reduced from 94.83 (10.36) to 90.36 (10.38) cm by the end of the intervention (P<.05). In contrast, the members of the control group only showed an improvement in their body mass index, waist measurement and body weight (P<.05). The mean waist measurement, body weight, blood pressure, and blood sugar level blood of the members of the treatment group were significantly lower than those of the controls (P<.05) (Table 1).
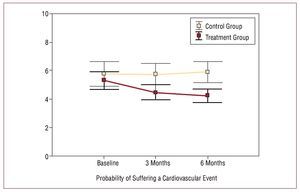
The changes made to the lifestyles of the subjects in the treatment group led to a reduction in their median (range) Framingham score from 5 (-10 to 12) to 3.5 (-11 to 10) (P<.05). In contrast, the score for the control group remained the same at 4. The probability of suffering a cardiovascular event within 10 years (mean [standard deviation]) was reduced from 5.29 (3.88) to 4.24 (2.86) (P<.05) among the treatment group subjects, but remained the same for the control group subjects (Figure 1).
Figure 1. Modification of the probability of suffering a cardiovascular event in the treatment and control groups (means [standard error]). Differences analyzed using the Friedman test (P<.05).
Some 63.16% of the treatment group subjects and 25.58% of the control subjects saw their cardiovascular risk reduced; some 10.53% and 34.88% respectively saw these increase (P<.05). The RR was 0.3 (95% CI, 0.11-0.83), the RRR was -69.8% (95% CI, -89 to -16.9), and the NNT was -5 (95% CI, -15 to -3). When adjusting for intention to treat, the RR obtained was 0.44 (95% CI, 0.20 to 0.96), the RRR was -56.3% (95% CI, -90.4% to -25,7%), and the NNT was -6 (95% CI, -13 to -3) (Table 2).
DISCUSSION
The present results show that the subjects who undertook lifestyle changes experienced a reduction in blood pressure, waist measurement and body weight, an improvement in their physical and aerobic condition, and were more likely to quit smoking. This agrees with that reported by Chobanian et al1 and the other experts of the JNC-VII who indicate that, in obese and overweight persons, weight reduction, a low-sodium DASH-type diet and physical activity are all useful in the prevention of high blood pressure and the reduction of cardiovascular risk.
The most significant effect of the present experimental program was the 10.6% reduction in systolic blood pressure and 12.9% reduction in diastolic blood pressure recorded - greater reductions than those reported achieved with a low sodium diet or weight reduction13 or a DASH diet alone.14 One third of the patients in the treatment group saw their blood pressure return to normal, an important result given that, according to Grotto et al,3 prehypertensive individuals have an RR for cardiovascular disease of 1.37-2.86.
The reduction achieved in body weight by the experimental program was significant, although smaller than that obtained by the Trials of Hypertension Prevention Collaborative Research Group over a 6 month period.14 This is explained in that the present program sought not only to achieve body weight loss but also to establish a general change in lifestyle in prehypertensive—but not necessarily obese nor overweight—individuals.
After 6 months of following the program, the members of the treatment group experienced reductions in the Framingham score (an absolute reduction of 1.5) and a percentage point drop in their likelihood of suffering a cardiovascular event within 10 years. Recently, Wister et al15 reported a greater reduction in primary and secondary care patients subjected to lifestyle change, although their study population included subjects with a cardiovascular risk of >10%.
The intervention program was effective in modifying the lifestyles of the treatment group members. Their lifestyle score increased by almost 30% compared to the 11% achieved with standard management. The FANTASTIC questionnaire is a validated instrument that was created to allow primary care physicians to assess the lifestyles of their patients. Other authors15 have assessed changes separately as a means of lifestyle assessment.
The present study investigates the effect of modifying lifestyle on cardiovascular risk (understood as a multidimensional variable that expresses the probability of suffering a cardiovascular event within 5 or 10 years), and examines how this probability can be modified over a short period (6 months), as recommended by the JNC-VII. When analyzing the cohort of subjects belonging to the Framingham study, Qureshi et al2 found that prehypertensive subjects were at greater risk of suffering a myocardial infarction and coronary artery disease. The results of the present study show that modifying lifestyle has a clear impact on cardiovascular risk in prehypertensive individuals, despite the fact that the Framingham score of the present subjects suggested them to be at low risk. This finding is important since prehypertension represents an early stage of high blood pressure during which attempts to change the clinical course of the disease could be effective. However, it should be remembered that the present study is subject to a number of limitations (which should be dealt with in future studies). For example, the sample size, although useful for determining the statistical significance of differences, may be too small to allow generalizations to be made regarding the entire population. Also, 17% of the members of the treatment group were lost to follow-up; even when correcting for intention to treat, this accentuated the sex difference between the groups. Further clinical trials or long-term cohort studies will be required to confirm the benefit of lifestyle changes on cardiovascular risk.
Correspondence: Dr. F.G. Márquez-Celedonio.
Laguna de Alvarado, 673. 91779 Veracruz. Veracruz. Mexico.
E-mail: felixg.marquez@imss.gob.mx
Received October 24, 2007.
Accepted for publication March 5, 2008.